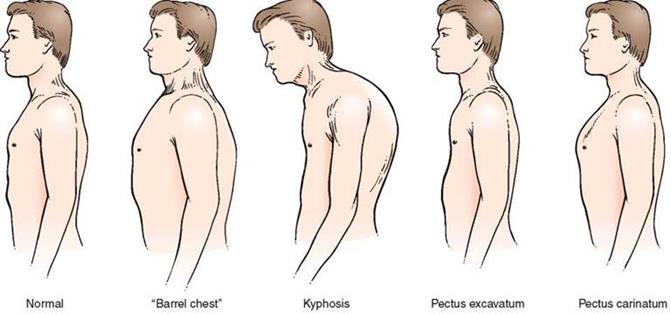
Form of the chest
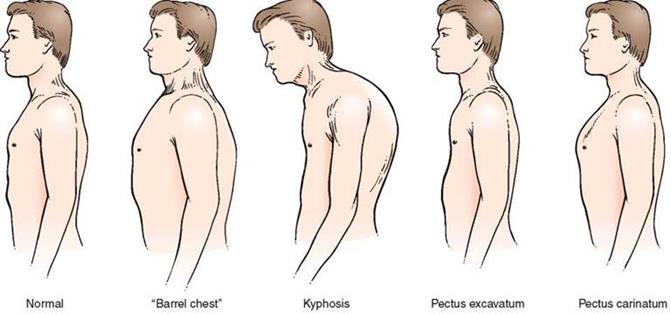
Normosthenic (conical) chest in subjects with normosthenic constitution resembles a truncated cone whose bottom is formed by well-developed muscles of the shoulder girdle and is directed upward. The anteroposterior (sternovertebral) diameter of the chest is smaller than the lateral (transverse) one, and the supraclavicular fossae are slightly pronounced. There is a distinct angle between the sternum and the manubrium (angulus Ludowici); the epigastric angle nears 90°. The ribs are moderately inclined as viewed from the side; the shoulder blades closely fit the chest and are at the same level; the chest is about the same height as the abdominal part of the trunk.
Hypersthenic chest in persons with the hypersthenic constitution has the shape of a cylinder. The anteroposterior diameter is about the same as the transverse one; the supraclavicular fossae are absent (level with the chest). The manubriosternal angle is indistinct; the epigastric angle exceeds 90°; the ribs in the lateral parts of the chest are nearly horizontal, the intercostal space is narrow, the shoulder blades are closely fit to the chest, 18 the thoracic part of the trunk is smaller than the abdominal one.
Asthenic chest in persons with the asthenic constitution is elongated, narrow (both the anteroposterior and transverse diameters are smaller than normal); the chest is flat. The supra- and subclavicular fossae are distinctly pronounced. There is no angle between the sternum and the manubrium: the sternal bone and the manubrium make a straight "plate". The epigastric angle is less than 90°. The ribs are more vertical at the sides, the tenth ribs are not attached to the costal arch (costa decima fluctuens); the intercostal spaces are wide, the shoulder blades are winged (separated from the chest), the muscles of the shoulder girdle are underdeveloped, the shoulders are sloping, the chest is longer than the abdominal part of the trunk.
Pathological chest
Emphysematous (barrel-like) chest resembles a hypersthenic chest in its shape, but differs from it by a barrel-like configuration, prominence of the chest wall, especially in the posterolateral regions, the intercostal spaces are enlarged. This type of chest is found in chronic emphysema of the lungs, during which elasticity of the lungs decreases while the volume of the lungs increases; the lungs seem to be as if at the inspiration phase. Natural expiration is therefore difficult not only during movements but also at rest (expiratory dyspnea is found). Active participation of accessory respiratory muscles in the respiratory act (especially m. sternocleidomastoideus and m. trapezius), depression of the intercostal space, the elevation of the entire chest during inspiration and relaxation of the respiratory muscles, and lowering of the chest to the initial position during expiration become evident during the examination of emphysema patients.
Paralytic chest resembles the asthenic chest. It is found in emaciated patients, in general asthenia and constitutional underdevelopment; it often occurs in grave chronic diseases, more commonly in pulmonary tuberculosis and pneumosclerosis, in which fibrous tissue contracts the lungs and diminishes its weight due to progressive chronic inflammation. During the examination of patients with paralytic chest, marked atrophy of the chest muscles and asymmetry of the clavicles, and dissimilar depression of the supraclavicular fossae can be observed along with typical signs of the asthenic chest. The shoulder blades are not at one level either, and their movements during breathing are asynchronous.
Rachitic chest (keeled or pigeon chest). It is characterized by a markedly greater anteroposterior diameter (compared with the transverse diameter) due to the prominence of the sternum (which resembles the keel of a boat.) The anterolateral surfaces of the chest look like they are pressed on both sides and therefore the ribs meet at an acute angle at the sternal bone, while the costal cartilages thicken like beads at points of their transition to bones (rachitic beads). As a rule, these beads can be palpated after rickets 19 only in children and youths.
Funnel chest can occur in normosthenic, hypersthenic or asthenic subjects; it has a funnel-shaped depression in the lower part of the sternum. This deformity can be regarded as a result of abnormal development of the sternum or prolonged compressing effect. In older times this chest would be found in shoemaker adolescents. The mechanism of formation of the funnel chest was explained by the permanent pressure of the chest against the shoe; the funnel chest was therefore formerly called the cobbler chest.
Foveated chest is almost the same as the funnel chest except that the depression is found mostly in the upper and the middle parts of the anterior surface of the chest. This abnormality occurs in syringomyelia, a rare disease of the spinal cord.
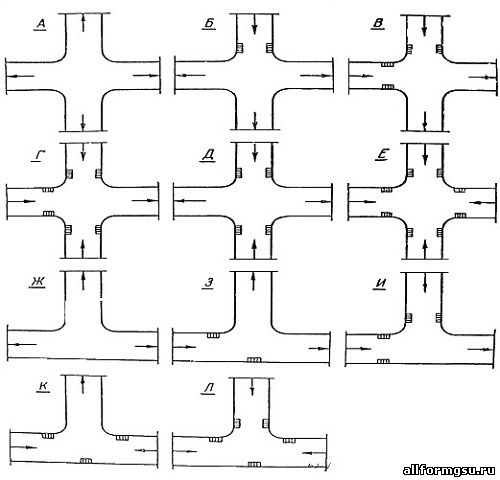
Picture 8. Examples of various chest shapes.
Spine deformities
The chest may be abnormal in subjects with various deformities of the spine which arise as a result of injuries, tuberculosis of the spine, rheumatoid arthritis (Bekhterev's disease), etc. Four types of spine deformities are distinguished: (1) lateral curvature of the spine, called scoliosis; (2) excessive-forward and backward curvature of the spine (gibbus and kyphosis, respectively); (3) forward curvature of the spine, generally in the lumbar region (lordosis); (4) combination of the lateral and forward curvature of the spine (kyphoscoliosis).
Scoliosis is the most frequently occurring deformity of the spine. It mostly develops in schoolchildren due to bad habitual posture. Kyphoscoliosis occurs less frequently. Lordosis only occurs in rare cases. The Curvature of the spine, especially kyphosis, lordosis, and kyphoscoliosis cause marked deformation of the chest to change the physiological position of the lungs and the heart and thus interfere with their normal functioning.
Asymmetry of the chest
The shape of the chest can readily change due to enlargement or diminution of one-half of the chest (asymmetry of the chest). These changes can be transient or permanent.
The enlargement of the volume of one-half of the chest can be due to the escape of considerable amounts of fluid as the result of inflammation (exudate) or non-inflammatory fluid (transudate) into the pleural cavity, or due to penetration of air inside the chest in injuries (pneumothorax). Leveling or protrusion of the intercostal spaces, asymmetry of the clavicles and the shoulder blades and also unilateral thoracic lagging can be observed during examination of the enlarged part of the chest. The chest assumes a normal shape after the air or fluid is removed from the pleural cavity.
One part of the chest may diminish due to (1) pleural adhesion or complete closure of the pleural slit after resorption of effusion (after the prolonged presence of the fluid in the pleural cavity); (2) contraction of a considerable portion of the lung due to growth of connective tissue 20 (pneumosclerosis) after acute or chronic inflammatory processes, such as acute lobar pneumonia (with subsequent carnification of the lung), lung infarction, pulmonary abscess, tuberculosis, etc.; (3) resection of a part of the entire lung; (4) atelectasis (collapse of the lung or its portion) that may occur due to closure of the lumen in a large bronchus by a foreign body or a tumor growing into the lumen of the bronchus and causing its obturation. The closure of the air passage into the lung with subsequent resorption of air from the alveoli and a decrease in the volume of the lung diminish the corresponding half of the chest. The chest thus becomes asymmetrical, the shoulder of the affected side lowers, the clavicle and the scapula lower as well, and their movements during deep respiration become slower and limited; the supra-and subclavicular fossae become more depressed, the intercostal spaces decrease in size or become invisible. The marked depression of the supraclavicular fossa on one side often depends on the diminution of the apex of a fibrosis-affected lung.
Dynamic survey of the chest
Respiratory movements of the chest should be examined during the dynamic survey of the chest. In physiological conditions, they are performed by the contraction of the main respiratory muscles: intercostal muscles, muscles of the diaphragm, and partly the abdominal wall muscles. The so-called accessory respiratory muscles (mm. sternocleidomastoideus, trapezius, pectoralis major et minor, etc.) are actively involved in the respiratory movements in pathological conditions associated with difficulty breathing.
The type, frequency, depth and rhythm of respiration can be determined by carefully observing the chest and the abdomen.
Respiration can be costal (thoracic), abdominal, or mixed type.
Thoracic (costal) respiration. Respiratory movements are carried out mainly by the contraction of the intercostal muscles. The chest markedly broadens and slightly rises during inspiration, while during expiration it narrows and slightly lowers. This type of breathing is known as costal and is mostly characteristic of women.
Abdominal respiration. Breathing is mainly accomplished by the diaphragmatic muscles; during the inspiration phase the diaphragm contracts and lowers to increase rarefaction in the chest and to suck in air into the lungs. The intra-abdominal pressure increases accordingly to displace the abdominal wall. During expiration the muscles are relaxed, the diaphragm rises, and the abdominal wall returns to the initial position. This type of respiration is also called diaphragmatic and is mostly characteristic of men.
Mixed respiration. The respiratory movements are carried out simultaneously by the diaphragm and the intercostal muscles. In 21 physiological conditions, this respiration sometimes occurs in aged persons and some pathological conditions of the respiratory apparatus and the abdominal viscera. For example, in women with dry pleurisy, pleural adhesion, myositis, and thoracic radiculitis, the contractile activity of the intercostal muscles decreases, and the respiratory movements are carried out by the accessory movements of the diaphragm. In extensive pleural adhesion, lung emphysema, and strong pain in the chest due to acute inflammation of the intercostal muscles or nerves, respiration is temporarily carried out by the diaphragmatic muscles exclusively. Mixed respiration occurs in men with underdeveloped diaphragmatic muscles, in diaphragmatitis, acute cholecystitis, perforating ulcer of the stomach or the duodenum. Respiration in such cases is sometimes carried out only by the intercostal muscles.
Respiration rate
Respiration rate can be determined by counting the movements of the chest or the abdominal wall, with the patient being unaware of the procedure. The pulse rate should first be taken and then the respiration rate. The number of respiratory movements in a healthy adult at rest should be 16 to 20 per minute, in the newborn 40-45, this rate gradually decreasing with age. The respiration rate decreases during sleep to 12—14 per minute, while under physical load, emotional excitement, or after heavy meals the respiration rate increases.
The respiration rate alters markedly in some pathological conditions. The causes of accelerated respiration may be (1) narrowing of the lumen of small bronchi due to spasms or diffuse inflammation of their mucosa (bronchiolitis occurring mostly in children), which interfere with normal passage of air into the alveoli; (2) decreased respiratory surface of the lungs due to their inflammation and tuberculosis, in collapse or atelectasis of the lung due to its compression (pleurisy with effusion, hydrothorax, pneumothorax, tumour of mediastinum), in obturation or compression of the main bronchus by a tumour, in thrombosis or embolism of the pulmonary artery, in pronounced emphysema, when the lung is overfilled with blood or in a case of lung edema in certain cardiovascular diseases; (3) insufficient depth of breathing (superficial respiration) which can be due to difficult contractions of the intercostal muscles or the diaphragm in acute pain (dry pleurisy, acute myositis, intercostal neuralgia, rib fracture, or tumour metastasis into the ribs), in a sharp increase in the intra-abdominal pressure and high diaphragm (ascites, meteorism, late pregnancy), and finally in hysteria.
Pathological deceleration of respiration occurs in functional inhibition of the respiratory center and its decreased excitability. It can be due to increased intracranial pressure in patients with cerebral tumor, meningitis, cerebral hemorrhage, or edema of the brain, and also due to the toxic effect on the respiratory center when toxic substances are 22 accumulated in the blood, e.g. in uremia, hepatic or diabetic coma, and in certain acute infectious diseases.
Respiration depth. The depth of breathing is determined by the volume of the inhaled and exhaled air at rest. This volume varies in an adult from 300 to 900 ml (500 ml on average). Depending on the depth, breathing can be either deep or superficial. Superficial (shallow) breathing often occurs in pathologically accelerated respiration when the length of the inspiration and the expiration phases becomes short. Deep breathing is, on the contrary, associated in most cases with a pathological deceleration of the respiration rate.
Deep and slow respiration, with marked respiratory movements, is sometimes attended by noisy sounds. This is Kussmaul's respiration occurring in a deep coma accompanied by decompensated acidosis (diabetic hyperglycemic-hyperketonemic coma, uremic coma). In some pathological conditions, however, rare respiration can be shallow, while accelerated breathing deep. Rare superficial respiration can occur in sharp inhibition of the respiratory center, pronounced lung emphysema, and sharp narrowing of the vocal slit or the trachea. Respiration becomes accelerated and deep in high fever and marked anemia.
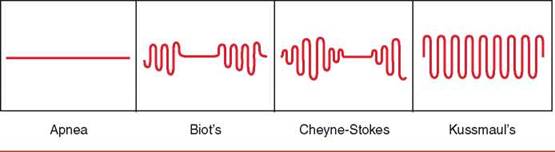
Respiration rhythm. The respiration of a healthy person is rhythmic, of uniform depth and equal length of the inspiration and expiration phases. The rhythm of the respiratory center can be inhibited in some types of cerebral edema. Derangement of the respiratory function can cause disorders in which a series of respiratory movements alternate with a pronounced (readily detectable) elongation of the respiratory pause (lasting from a few seconds to a minute) or a temporary arrest of respiration (apnea). This respiration is known as periodic respiration.
Biot's respiration is characterized by rhythmic but deep respiratory movements which alternate (in approximately regular intervals) with long respiratory pauses (from few seconds to half a minute). Biot's respiration occurs in meningitis patients and in agony with disorders of cerebral circulation.
Cheyne-Stokes respiration is characterized by periods (from few seconds to a minute) of cessation of respiration, followed by noiseless shallow respiration, which quickly deepens, becomes noisy to attain its maximum at the 5-7th inhalation, and then gradually slows down to the end with a new short respiratory pause. During such pauses, the patient often loses his sense of orientation in the surroundings or even faints, to recover from the unconscious condition after respiratory movements are restored. This respiratory disorder occurs in diseases causing acute or chronic insufficiency of the cerebral circulation and brain hypoxia, and also in heavy poisoning. More frequently this condition develops during sleep and is more characteristic of aged persons with marked atherosclerosis of the cerebral arteries.
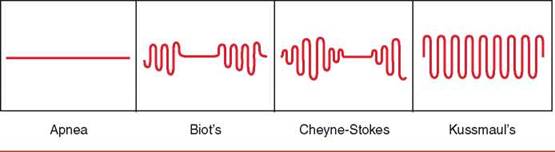
Picture 9. Pathologic respiration rhythm
Undulant (wave-like) Grocco's respiration somewhat resembles Cheyne-Stoke's respiration except that weak shallow respiration occurs instead of the respiratory pause with subsequent deepening of the respiratory movement, followed by slowing down. This type of arrhythmic dyspnea can probably be regarded as the early stages of the same pathological processes which responsible for Cheyne-Stokes respiration.
Palpation of the chest
Palpation is used as an additional means of examination to verify findings of observation (the shape of the chest, its dimensions, respiratory movements), for determining local or profuse tenderness of the chest, its elasticity (resistance), vocal fremitus, pleural friction and sounds of fluid in the pleural cavity.
Palpation should be done by placing the palms on the symmetrical (left and right) parts of the chest. This examination helps follow the respiratory excursions and deviation of the chest movements from their normal course. The epigastric angle is determined by palpation as well. The thumbs should be pressed tightly against the costal arch, their tips resting against the xiphoid process.
Palpation is used to locate pain in the chest and its irradiation. For example, in rib fracture, pain is localized over a limited site, namely at the point of the fracture. Displacement (careful) of bone fractures will be attended in this case by a specific sound (crunch). Inflammation of the intercostal nerves and muscles also causes pain, but it can be felt during palpation over the entire intercostal space. Such pain is called superficial. It is intensified during deep breathing when the patient bends to the affected side or lies on this side.
Resistance (elasticity) of the chest is determined by exerting pressure of the examining hands from the front to the sides of the chest or on the back and the sternum, and also by palpation of the intercostal spaces. The chest of a healthy person is elastic. The chest of a healthy person may be compressed on 2-3 cm under moderate pressure in both the anteroposterior and lateral directions. In the presence of pleurisy with effusion or pleural tumor, the intercostal space over the affected site becomes rigid. The rigidity of the chest increases in general in the aged due to ossification of the costal cartilages, development of the lung emphysema, and also the filling of both pleural cavities with fluid. Increased resistance of the chest can be felt during examining the chest by compression in both the anteroposterior and lateral directions.
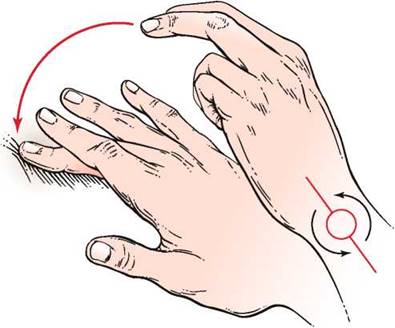
Palpation is used for determining the strength of voice conduction to the chest surface (fremitus vocalis s. pectoralis). The palms of the hands are placed on the symmetrical parts of the chest and the patient is asked to utter 24 loudly a few words (with the letter 'r' in them to intensify vibration). The voice should be as low as possible since voice vibrations are better transmitted by the air column in the trachea and the bronchi to the chest wall in this case. Fremitus vocalis can also be determined by one hand as well: the palm of the examining hand should be placed alternately on the symmetrical parts of the chest. Fremitus vocalis is not determined at the region of the heart below the third rib on the left parasternal and midclavicular lines.
Vocal fremitus is of about the same intensity in the symmetrical parts of the chest of a healthy person. Vocal vibrations are louder in the upper parts of the chest and softer in its lower parts. Moreover, voice conduction is better in men with a low voice and thin chest; the vibrations are weaker in women and children with higher voice (and also in persons with well-developed subcutaneous fat tissues). Vocal fremitus can be stronger or weaker (or in some cases it can even be impalpable) in pathological conditions of the respiratory organs. In focal affections, the vocal fremitus becomes unequal over symmetrical parts of the chest.
Vocal fremitus is intensified when a part of the lung or its whole lobe becomes airless and more uniform (dense) because of a pathological process. According to the laws of physics, dense and uniform bodies conduct sound better than loose and non-uniform. Induration (consolidation) can be due to various causes, such as acute lobar pneumonia, pulmonary infarction, tuberculosis, accumulation of air or fluid in the pleural cavity, etc. Vocal fremitus is also intensified in the presence in the pulmonary tissue of an air cavity communicated with the bronchus.
Vocal fremitus- becomes weaker (1) when liquid or gas are accumulated in the pleural cavity; they separate the lung from the chest wall to absorb voice vibrations propagating from the vocal slit along the bronchial tree; (2) in case of full obstruction of the bronchial lumen by a tumor which interferes with the normal conduction of sound waves to the chest wall; (3) in asthenic emaciated patients (with weak voice); (4) In severe thickening of the chest wall in obesity.
Low-frequency vibrations due to pleural friction (friction fremitus) in dry pleurisy, crepitation sounds characteristic of subcutaneous emphysema of the lungs, vibration of the chest in dry, low (low-pitch buzzing) rales can also be determined by palpation.
Percussion of lungs
Percussion (L percutere to strike through) was first proposed by an Austrian physician Auenbrugger in 1761. Tapping various parts of the human body produces sounds by which one can learn about the condition of 25 the underlying organs. The organs or tissues lying beneath the percussing area begin vibrating and these vibrations are transmitted to the surrounding air whose vibration is perceived by our ears as sounds. Liquids and airless tissues give dull sounds which can be heard with difficulty, such as the sound of a percussed femur (femoral sound). Airless organs and also liquids cannot therefore be differentiated by percussion. The properties of each particular sound obtained by percussion of the chest or the abdomen, and differing from the femoral sound, depending on the amount of air or gas enclosed within the chest or abdomen. The difference in the sounds of percussed lungs, liver, spleen, heart, stomach and other organs depends on (a) the different amount of gas or air inside or round the percussed organ; (b) tension of the tissue; and (c) different strength of the percussion stroke transmitted to this gas or air.
Mediate percussion is done by tapping with a plexor (hammer) on a pleximeter placed on the body, or by a finger on another finger. In immediate percussion, the examined part of the body is struck directly by the soft tip of the index finger. To make tapping stronger, the index finger may be first held by the side of the middle finger and then released. This method was proposed by Obraztsov. Its advantage is that the striking finger feels the resistance of the examined part of the body.
Picture 10. Technique of percussion
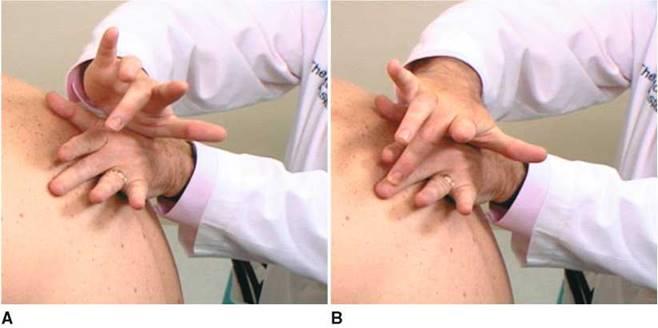
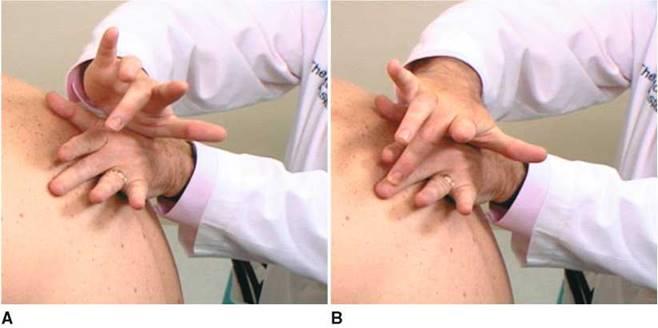
Picture11. A, Position of the right hand ready to percuss. B, Location of the fingers after striking. Notice that the motion is from the wrist.
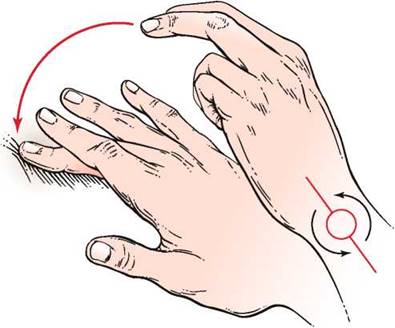
Percussion is done with a slightly flexed middle finger on the dorsal side of the second phalanx of the middle finger of the opposite hand, which is pressed tightly against the examined part of the body. Percussion should be done by the movement of the wrist alone without involving the forearm in the movement. Striking intensity should be uniform, blows must be quick and short, directed perpendicularly to the intervening finger. Tapping should not be strong.
Sounds obtained by percussion differ in strength (clearness), pitch, and tone. Sounds may be strong and clear (resonant) or soft and dull; they may be high or low, and either tympanic or non-tympanic (and with metallic tinkling).
Resonance (clearness, loudness, sound volume) of the percussion sound largely depends on the vibration amplitude: the stronger the tapping the louder is the sound; uniform strength of tapping is therefore required. A louder sound will be heard during the percussion of an organ containing a greater amount of air. In healthy persons, resonant and clear sounds are heard in the percussion of thoracic and abdominal organs filled with gas or air (lungs, stomach, and intestine).
Soft or dull sound is heard during percussion of the chest and the abdominal wall overlying airless organs (liver, heart, spleen), and also during percussion of muscles (femoral sound). Resonant and clear sound will become soft if the amount of air decreases inside the lung or if the liquid is accumulated between the lungs and the chest wall (in the pleural cavity).
The pitch of the sound depends on the vibration frequency: the smaller the volume of the examined organ, the higher the vibration frequency, hence the higher the pitch. Percussion of healthy lungs in children gives higher sounds than in adults. The sound of a lung containing excess air (emphysema) is lower than that of a healthy lung. This sound is called bandbox (box sound). The normal vibration frequency of a healthy lung during percussion is 109-130 per second, while in emphysema the frequency decreases to 70-80 c/s. Quite the opposite, if the pulmonary tissue becomes more consolidated, the frequency increases to 400 c/s and more.
Tympanic sound resembles the sound of a drum (hence its name: Gk tympanon drum). Tympany differs from a non-tympanic sound by higher regularity of vibrations and therefore it approaches a musical tone, while a non-tympanic sound includes many aperiodic vibrations and sounds like noise. A tympanic sound appears when the tension in the wall of an air-containing organ decreases. Tympany can be heard during percussion of the stomach and the intestine of healthy people. Tympany is absent during percussion of healthy lungs, but if the tension in the pulmonary tissue decreases, tympanic sounds can be heard. This occurs in incomplete compression of the lung by the pleural effusion, in inflammation or edema of the lung (the percussion sound then becomes dull tympanic). A tympanic sound can also be heard if air cavities are formed in the lungs or when air penetrates the pleural cavity. Tympany is heard over large caverns and in open pneumothorax (the sound is resonant). Since air-filled organs produce resonant percussion sounds and airless organs give dull sounds, the difference between these sounds helps locate the borders between these organs (e.g. between the lungs and the liver, the lungs and the heart, etc.).
Topographic percussion is used to determine the borders, size and shape of organs. Comparison of sounds on symmetrical points of the chest is called comparative percussion.
Tapping strength can vary depending on the purpose of the examination. Loud percussion (with a normal force of tapping), light (quiet), and lightest (quietest, threshold) percussion are differentiated. The heavier the percussion stroke, the greater is the area and depth to which the tissues are set vibrating, and hence the more resonant is the sound. In heavy or deep percussion, tissues lying at a distance of 4- 7 cm from the pleximeter are involved. In light or surface percussion the examined zone has a radius of 2—4 cm. Loud percussion should therefore be used to examine deeply located organs, and light percussion - for examining superficial organs. Light percussion is used to determine the size and borders of various organs (liver, lungs and heart).
Main rules of percussion
1. The patient should be in a comfortable posture and relaxed. The best position is standing or sitting. Patients with grave diseases should be 27 percussed in the lying position. When the patient is percussed from his back, he should be sitting on a chair, his face turned to the chair back. The head should be slightly bent forward; his arms should rest against his lap. In this position muscle relaxation is the greatest and percussion thus becomes easier.
2.The room should be warm and protected from external noise.
3.The physician should be in a comfortable position as well.
4.A pleximeter or the middle finger of the left hand, which is normally used in the finger-to-finger percussion, should be pressed tightly to the examined surface. The neighboring fingers should be somewhat set apart and tightly pressed to the patient's body. This is necessary to delimit the propagation of vibrations arising during percussion. The physician's hands should be warm.
5.The percussion sound should be produced by the tapping movement of the hand alone. The sound should be short and distinct. Tapping should be uniform, the force of percussion strokes depending on the object being examined (see above).
6.In topographic percussion, the finger-pleximeter should be placed parallel to the anticipated border of the organ. Organs giving resonant notes should be examined first: the ear will better detect changes in sound intensity. The border is marked by the edge of the pleximeter directed toward the zone of the more resonant sounds.
7.Comparative percussion should be carried out on exactly symmetrical parts of the body.
Percussion of lungs. Depending on the object of examination, various methods of percussion are used to examine the lungs. The examination begins with comparative percussion.
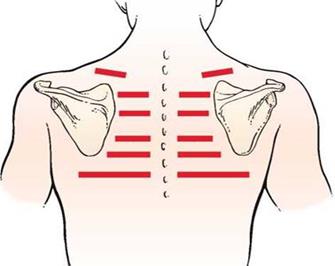
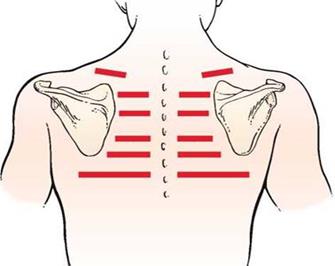
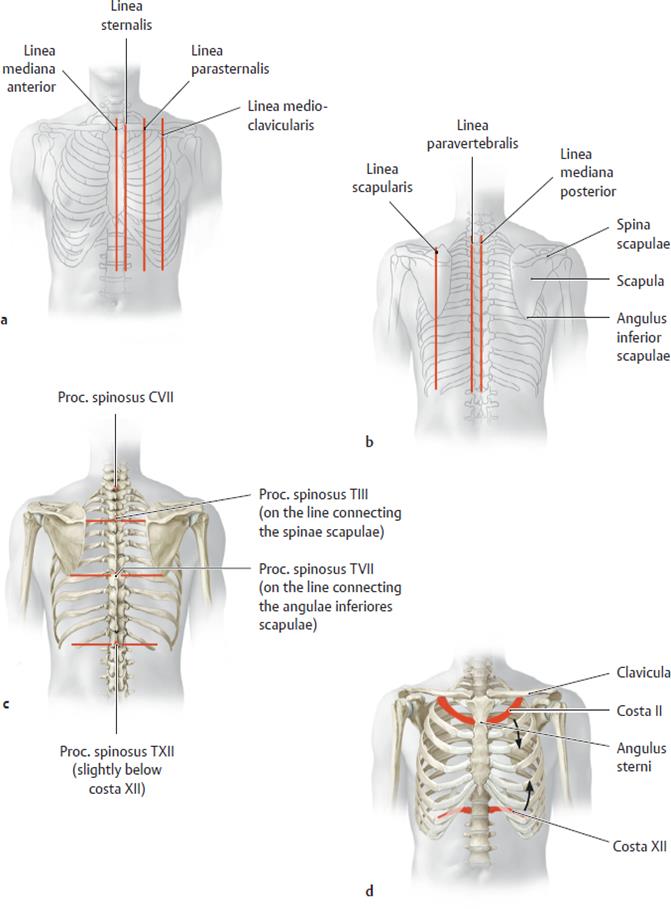
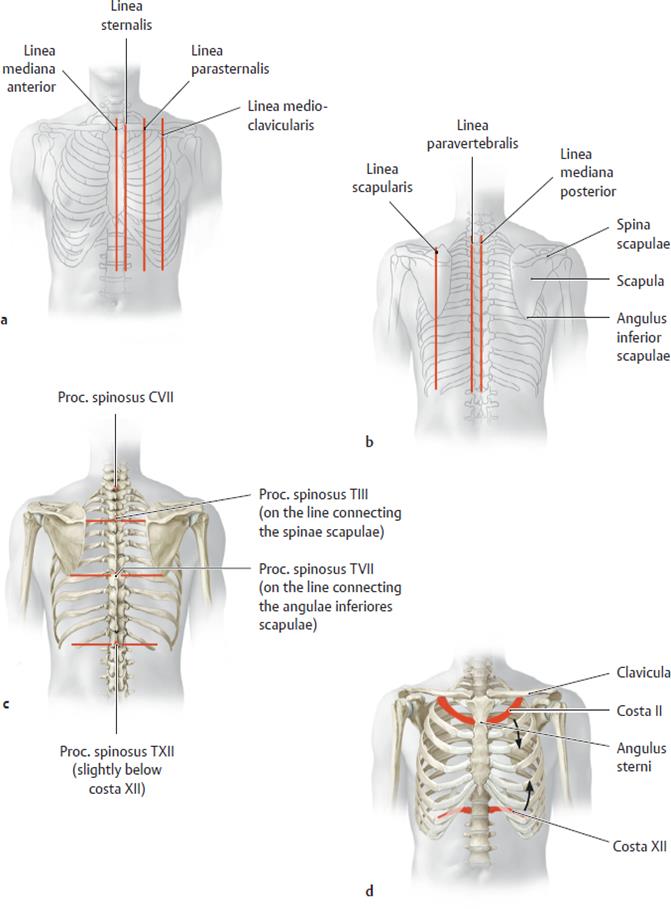
Picture12. Locations on the posterior (left) and anterior (right) chest for percussion and auscultation
Comparative percussion is performed to a comparison of the percussion sound (resonance) on the symmetrical points of the appropriate topographical lines of the chest.
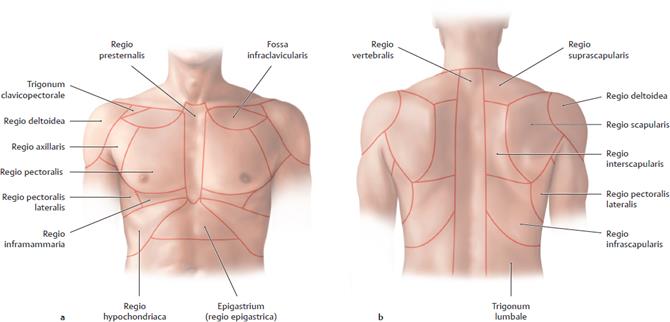
A certain sequence is followed in comparative percussion. Percussion sounds over the lung apices (in the front) on the symmetrical points of the chest are first compared; the pleximeter finger is placed parallel to the clavicle. The plexor finger is then used to strike the clavicle which is used as a pleximeter in this case. During percussion of the lungs below the clavicle, the pleximeter finger is placed in the interspace at the strictly symmetrical points of the left and right sides of the chest. The percussion sounds are compared only to the level of the 3rd rib along the parasternalis line and to the level of the 4th rib along the midclavicular line (further the percussion is continued only on the right side of the chest to hepatic dullness). The heart lying below this level changes the percussion sound. For comparative percussion of the axillary region, the patient should raise his arms and clamp the hands at the back of the head. Comparative percussion of the lungs on the back begins with suprascapular areas. The pleximeter finger is placed horizontally, while during percussion of the regions between the scapulae, the pleximeter should be vertical. The patient should cross his arms on the chest to displace the scapulae anteriorly (away from the backbone). During percussion of the points lying below the scapulae, the pleximeter should again be horizontal; in the interspace, it should be placed parallel to the ribs.
Percussion sounds of the lungs of a healthy person cannot be of equal strength, length or pitch even if the percussion blows are uniform at symmetrical points. This depends on the mass and thickness of the pulmonary layer and also on the influence of the adjacent organs on the percussion sound. It is softer and shorter (1) over the right upper lobe because it is located somewhat below the left (due to the shorter right upper bronchus) and also because of the better development of the muscles of the appropriate 29 side of the shoulder girdle; (2) in the second and third interspace on the left, because of the closer location of the heart; (3) over the upper lobes of the lung (compared with the lower lobes) because of the varying thickness of pneumatic pulmonary tissue; (4) in the right axillary region (compared with the left one) because of the closer location of the liver. The difference in percussion sounds here depends on the fact that the diaphragm and the lung border on the left with the stomach whose bottom is filled with air and gives a loud tympanic sound during percussion (Traube's semilunar space). The percussion sound in the left axillary region is, therefore, louder and higher (with the tympanic character) because of the resonant effect (“air bladder”) of the stomach.
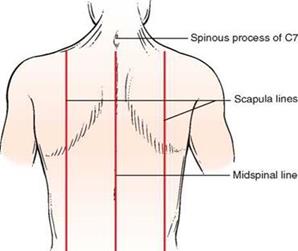
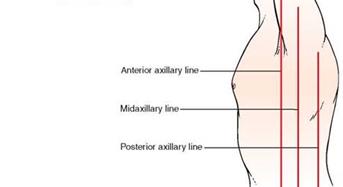
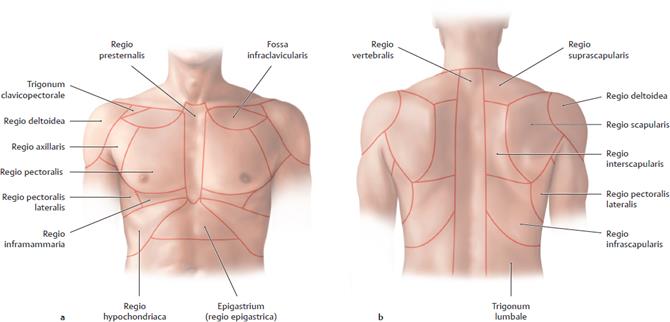
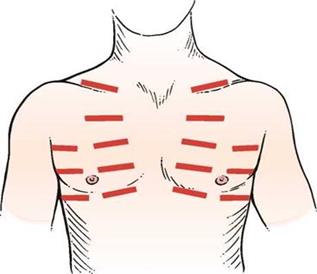
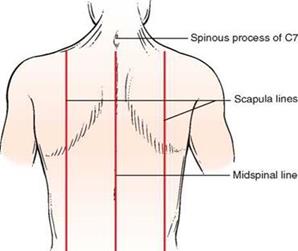
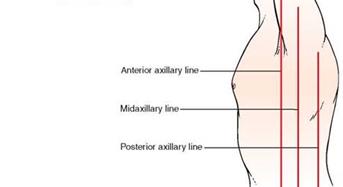
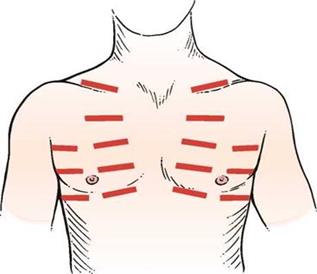
Picture13. Topographic lines and regions of the chest
Picture14. Topographic lines and identification points on the chest
The percussion sound can change in pathological processes because of the decreased content or full absence of air in a part of the lung, and because of the pleural fluid (transudate, effusion, blood), increased airiness of the lung tissue, and the presence of air in the pleural cavity (pneumothorax).
The amount of air in the lungs decreases in (1) pneumosclerosis, fibrous-focal tuberculosis, (2) pleural adhesion or obliteration of the pleural cavity which interferes with normal distention of the lung during inspiration; the difference in the percussion sound will be more pronounced at the inspiration level and weaker during the expiration; (3) lobular and especially confluent pneumonia, in which pulmonary tissue alternates with consolidations; (4) considerable edema of the lungs, especially in the inferiolateral regions due to insufficient contractility of the left ventricle; (5) compression of the pulmonary tissue by the pleural fluid (compression atelectasis) above the fluid level; (6) complete obstruction of the large bronchus with a tumor and gradual resorption of air from the lungs below the closure of the lumen (obstructive atelectasis). Clear pulmonary sounds become shorter and higher (i.e. duller) in the mentioned pathological conditions. If these conditions are attended by decreased tension in the elastic elements of the pulmonary tissue, e.g. in the presence of compression or obstructive atelectasis, the sound over the atelectatic zone becomes dull with a tympanic tone. This sound can also be heard during percussion of a patient with acute lobar pneumonia at its first stage, when the alveoli of the affected lobe, in addition to air, contain also a small amount of fluid.
A complete absence of air in the entire lobe of the lung or its part (segment) is observed in the following cases: (a) acute lobar pneumonia at the consolidation stage, when the alveoli are filled with the inflammatory exudate containing fibrin; (b) formation in the lung of a large cavity, which is filled with the inflammatory fluid (sputum, pus, echinococcus cysts, etc.), or heterogeneous airless tissue (tumor); (c) accumulation of fluid in the pleural cavity (transudate, exudate, blood). Percussion over airless parts of the lung or fluid accumulated in the pleural cavity gives a soft short and high sound which is called dull or, by analogy with the percussion sounds of 30 airless organs and tissues (liver, muscles), liver dullness. But the absolute dullness identical to the percussion sound of the liver can only be heard in the presence of a large amount of fluid in the pleural cavity
The amount of air in the lung increases in emphysema. The percussion sound in lung emphysema is louder than the dull tympanic sound because of the increased airiness of the pulmonary tissue and decreased elasticity of the tense pulmonary tissues, but the tympanic character is preserved. The percussion sound resembles the one produced by a stroke on a box; hence the name bandbox sound.
The amount of air held inside the lung increases with the formation of a smooth-wall cavity filled with air and communicated with the bronchus (abscess, tuberculosis cavern). The percussion sound over this area will be tympanic. If the cavity is small and situated deeply in the chest, vibrations of the pulmonary tissue will not reach this cavity and no tympanic sound will be heard. Such a cavity will only be revealed by roentgenoscopy. The sound over a very large smooth-wall cavity in the lung (6—8 cm in diameter) will be tympanic, resembling a stroke on a metal (metallic percussion sound). If this cavity is located superficially and is communicated with the bronchus through a narrow slit, the percussion sound will be soft and will resemble that of a cracked pot (hence the name - cracked-pot sound).
Auscultation of the lungs
Auscultation of the lungs should be performed according to a plan. A stethoscope or phonendoscope should be placed in strictly symmetrical points of the right and left sides of the chest. Auscultation begins with the anterior wall of the chest, from its upper part, in the supra- and subclavicular regions, and then the stethoscope should be moved downward and laterally. The lungs are then auscultated in the same order from the posterior wall of the chest and in the axillary regions. In order to increase the area of auscultation between the scapulae, the patient should be asked to cross his arms on the chest and in this way to displace his shoulder-blades laterally from the spine, while for convenience of auscultation of the axillary regions he should place his hands on the back of the head.
The posture does not matter, but the patient should better sit up on a stool with his hands on the lap. The patient may stand, but the physician should remember that deep breathing (hyperventilation of the lungs) may cause vertigo and the patient may faint. Bearing this in mind, and also to ensure tight contact between the stethoscope and the skin (especially if a one-piece stethoscope is used) the physician should always use his free hand to support the patient on the side opposite to the point of application of the stethoscope bell.
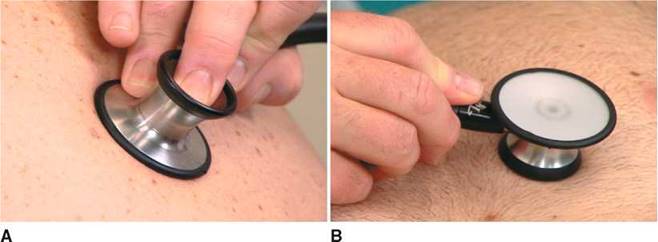
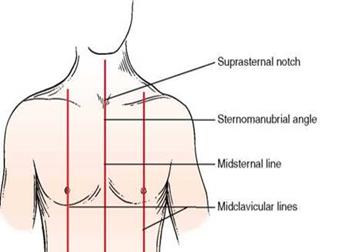
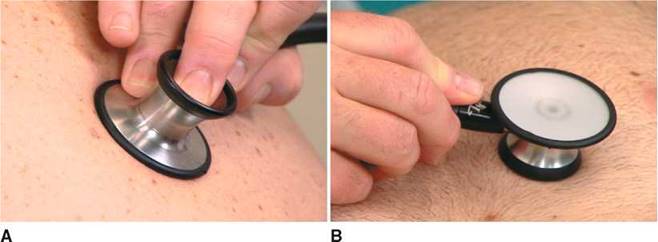
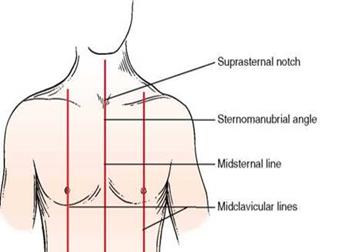
Picture 15.Placement of stethoscope heads. A, Correct placement of the diaphragm. Notice that the head is applied tightly to the skin. B, Placement of the bell. Notice that the bell is applied lightly to the skin.
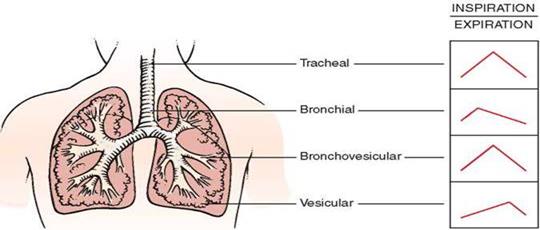
Respiratory murmurs (breath sounds) during various phases of respiration are first compared during auscultation of the lungs as well as their character, length, and intensity (loudness). Then these sounds are compared with the respiratory murmurs at the symmetrical points of the other half of the chest (comparative auscultation). Attention should be paid to the main respiratory sounds, such as vesicular (alveolar) breathing which is heard over the pulmonary tissues, and bronchial (laryngotracheal) breathing which is heard over the larynx, trachea, and large bronchi.
In the presence of pathology in the airways, in the alveolar tissue, or the pleura, adventitious sounds such as rales, crepitation, and pleural friction are heard in addition to the main breath sounds during inspiration and expiration. These adventitious sounds should be examined only after the character of the main sounds has been established. Normal breathing sounds should be better auscultated with nasal breathing (with the patient's mouth closed) while adventitious sounds are better heard with deep respiration through the open mouth.
Vesicular breathing (vesicular/ alveolar respiration)
Respiratory sounds known as vesicular respiration arise due to vibration of the elastic elements of the alveolar walls during their filling with air in inspiration. The alveoli are filled with air in sequence. Therefore, the summation of the great number of sounds produced during vibration of the alveolar walls gives a long soft (blowing) noise that can be heard during the entire inspiration phase, its intensity gradually increasing. This sound can be simulated by pronouncing the sound “T” during inspiration, or by drawing tea from a saucer. Alveolar walls still vibrate at the initial expiration phase to give a shorter second phase of the vesicular breathing, which is heard only during the first third of the expiration phase, because vibrations of elastic alveolar walls are quickly dampened by the decreasing tension of the alveolar walls.
Normal vesicular breathing is better heard over the anterior surface of the chest, below the 2nd rib, laterally of the parasternal line, and also in the axillary regions and below the scapular angle, i.e. at points where the largest masses of the pulmonary tissue are located. Vesicular breathing is heard worse at apex of the lungs and their lowermost parts, where the masses of the pulmonary tissue are less abundant. While carrying out comparative auscultation, it should be remembered that the expiration sounds are louder and longer in the right lung due to better conduction of the laryngeal sounds by the right main bronchus, which is shorter and wider. The respiratory sound sometimes becomes bronchovesicular over the right apex, or it may be mixed due to the more superficial and horizontal position of the right apical bronchus.
Alterations in vesicular respiration
Vesicular breathing can vary, i.e. it may be louder or softer for both physiological and pathological reasons.
Physiological weakening of vesicular respiration occurs in patients with thicker chest walls due to excessively developed muscles or subcutaneous fat. Physiological intensification of vesicular respiration may be observed in patients with underdeveloped muscles or subcutaneous fat. Intensified vesicular breathing is characteristic of children with a thin chest wall, good elasticity of the alveoli, and the interalveolar septa. This respiration is called “puerile respiration” (L puer child). Vesicular respiration is intensified during exercise; respiratory movements become deeper and more frequent. Physiological changes in vesicular respiration always involve both parts of the chest, and respiratory sounds are equally intensified or weakened at the symmetrical points of the chest.
In pathology, alterations in vesicular breathing maybe both uni- and bilateral, or else only over one lobe of the lung. Respiratory sounds become weaker or inaudible at all, or they may be intensified. Alterations in vesicular respiration in such cases depend on the number of intact alveoli and the properties of their walls, the amount of air contained in them, on the length 39 and strength of the expiration and inspiration phases, and finally on the conditions of sound conduction from the vibrating elastic elements of the pulmonary tissue to the surface of the chest.
Pathologically decreased vesicular respiration can be due to a significantly diminished number of the alveoli because of atrophy and gradual degradation of the interalveolar septa and formation of larger vesicles incapable of collapsing during expiration. This pathological condition is observed in pulmonary emphysema, at which the remaining alveoli are no longer elastic; their walls become incapable of quick distention and do not give sufficiently strong vibrations.
Decreased vesicular breathing can be due to inflammation and swelling of the walls in a part of the lung and decreased amplitude of their vibration during inspiration, which is characteristic of early acute lobar pneumonia. During the second stage of this disease, the alveoli of the affected part of the lung become filled with effusion and vesicular breathing becomes inaudible over this region. Vesicular breathing can be decreased also in insufficient delivery of air to the alveoli through the airways because of their mechanical obstruction (e.g. by a tumor). Air admission to the alveoli can be decreased in patients with a markedly weakened inspiration phase (as a result of inflammation of the respiratory muscles, intercostal nerves, rib fracture, extreme asthenia of the patient and adynamia).
Vesicular respiration decreases also due to obstructed conduction of sound waves from the source of vibration (alveolar walls) to the chest surface, as, for example, in thickening of the pleural membranes or accumulation of air or fluid in the pleural cavity. If the amount of fluid or air in the pleural cavity is great, respiratory sounds are not heard. Conduction of sound to the surface of the chest may be absent in the atelectasis of the lung due to complete obstruction of the lumen in the large bronchus.
Abnormally increased vesicular respiration can be heard during expiration or during both respiratory phases. Increased expiration depends on obstruction to the air passage through small bronchi or their contracted lumen (inflammatory edema of the mucosa, bronchospasm). Expiration becomes louder and longer.
Deeper vesicular respiration during which the inspiration and expiration phases are intensified is called harsh (or coarse, rough) respiration. It occurs in marked and non-uniform narrowing of the lumen in small bronchi and bronchioles due to inflammatory edema of their mucosa (bronchitis).
Another type of pathological respiration is interrupted or cogwheel respiration. This vesicular respiration is characterized by short jerky inspiration efforts interrupted by short pauses between them; the expiration is usually normal. Interrupted breathing also occurs in a non-uniform contraction of the respiratory muscles, e.g. when a patient is auscultated in a cold room, 40 or when he has nervous trembling, or diseases of the respiratory muscles, etc. Interrupted breathing over a limited part of the lung indicates difficult passage of air from small bronchi to the alveoli in this region and uneven unfolding of the alveoli. Interrupted breathing indicates pathology in fine bronchi and is more frequently heard at the apices of the lungs during their tuberculosis infiltration.
Bronchial breathing/respiration (laryngotracheal respiration)
Respiratory sounds known as bronchial or tubular breathing arise in the larynx and the trachea as air passes through the vocal slit. As air is inhaled, it passes through the vocal slit to enter the wider trachea where it is set in vortex-type motion. Sound waves thus generated propagate along the air column throughout the entire bronchial tree. Sounds generated by the vibration of these waves are harsh. During expiration, air also passes through the vocal slit to enter a wider space of the larynx where it is set in a vortex motion. But since the vocal slit is narrower during expiration, the respiratory sound becomes louder, harsher and longer. This type of breathing is called laryngotracheal (by the site of its generation).
Bronchial breathing is well heard in physiological cases over the larynx, the trachea, and at points of projection of the tracheal bifurcation (anteriorly, over the manubrium sterni, at the point of its junction with the sternum, and posteriorly in the interscapular space, at the level of the 3rd and 4th thoracic vertebrae). Bronchial breathing is not heard over the other parts of the chest because of large masses of the pulmonary tissue found between the bronchi and the chest wall.
Bronchial breathing can be heard instead of vesicular (or in addition to the vesicular breathing) over the chest in pulmonary pathology. This breathing is called pathological bronchial respiration.
It is conducted to the surface of the chest wall only under certain conditions, the main one being the duration of the pulmonary tissue when the alveoli are filled with effusion (acute lobar pneumonia, tuberculosis, etc.), with blood (lung infarction), or due to compression of the alveoli by air or fluids accumulated in the pleural cavity, and compression of the lung against its root (compression atelectasis). In such cases, the alveolar walls do not vibrate, while consolidated airless pulmonary tissue becomes a good conductor of sound waves in laryngotracheal respiration to the surface of the chest wall. Lungs may be consolidated due to the replacement of the inflated pulmonary tissue by connective tissue (pneumosclerosis, carnification of the lung lobe, which sometimes occurs in acute lobar pneumonia, etc.).
Depending on the degree of induration, its size and location in the lung, pathological bronchial breathing may have different intensity and pitch. If induration is large and superficial, loud bronchial breathing is heard as if near the ear. Bronchial breathing can be heard in acute lobar pneumonia at its 41-second stadium (affection of the entire lobe of the lung). Especially soft and low sounds are heard in patients with compression atelectasis.
Pathological bronchial breathing can be heard if an empty cavity is formed in the lung (abscess, cavern) and it is communicated with the bronchus. Consolidation of pulmonary tissue around the focus facilitates the conduction of sound waves of laryngotracheal respiration to the surface of the chest wall, the more so that sound is intensified in the resonant cavity at the moment of the air passage from narrow bronchus the air is set in vortex motion.
Depending on the origin there are three types of pathological bronchial respiration:
1) Infiltrative type arises in the consolidation of a pulmonary tissue (II stages of acute lobar pneumonia, infarct of lungs, tuberculosis),
2) Cavitary type is auscultated above superficially posed smooth-bore lumen of the big diameter connected with a bronchus (an abscess, a tubercular cavern, bronchiectasis with an appreciable distention of bronchi),
3) Atelectatic type - it is observed in compression atelectasis (exudative pleurisy of 1,5-3 liters), it is auscultated at a column on high bound of a dullness at place where lung is compressiated, rarely passes for lin. axillaries anterior.
Amphoric respiration arises in the presence of a smooth-wall cavity (not less than 5-6 cm in diameter) communicated with a large bronchus. Sounds of this kind can be produced by blowing over the mouth of an empty glass or clay jar. This altered bronchial breathing is there called amphoric.
Metallic respiration differs from both bronchial and amphoric. It is loud and high and resembles the sound produced when a piece of metal is struck. Metallic respiration is heard in open pneumothorax when the air of the pleural cavity communicates with external air.
Stenotic respiration is exaggerated laryngotracheal breathing which is heard in cases with narrowed trachea or large bronchus (due to a tumor); it is heard mainly at points where physiological bronchial breathing is normally heard.
Bronchovesicular or mixed respiration is heard in lobular pneumonia or infiltrative tuberculosis, and also in pneumosclerosis, with foci of consolidated tissue being seated deeply in the pulmonary tissue and far from one another. Mixed breathing, when the inspiration phase is characteristic of vesicular breathing and the expiration phase of bronchial breathing, is often heard in such cases instead of weak bronchial breathing.
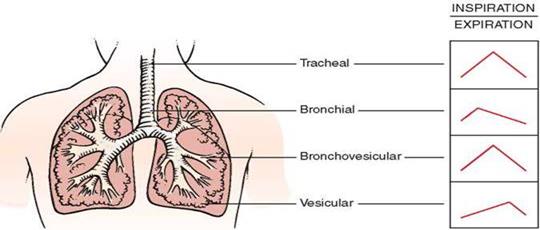
Picture 16. Characteristics of breath sounds.
Adventitious sounds (additional respiratory sounds)
Adventitious sounds are rales, crepitation, and pleural friction.
Rales arise in the pathology of the trachea, bronchi, or if a cavern is formed in the affected lung. Rales are classified as dry (rhonchi) and moist rales. Dry rales, or rhonchi, may be due to various causes. The main one is the constriction of the lumen in the bronchi. Constriction may be total (in bronchial asthma), non-uniform (in bronchitis), or focal (in tuberculosis or tumor of the bronchus). Dry rales can be due to (1) spasms of smooth muscles of the bronchi during attacks of bronchial asthma; (2) swelling of the bronchial mucosa during its inflammation; (3) accumulation of viscous sputum in the bronchi which adheres to the wall of the bronchus and narrows its lumen; (4) formation of fibrous tissue in the walls of separate bronchi and in the pulmonary tissue with subsequent alteration of their architectonics (bronchiectasis, pneumosclerosis); (5) vibration of viscous sputum in the lumen of large and medium-size bronchi during inspiration and expiration: being viscous, the sputum can be drawn (by the air stream) into threads which adhere to the opposite walls of the bronchi and vibrate like strings.
Moist rales are generated because of the accumulation of liquid secretion (sputum, edematous fluid, blood) in the bronchi through which air passes. Air bubbles pass through the liquid secretion of the bronchial lumen and collapse to produce a specific cracking sound. This sound can be simulated by bubbling air through water using a fine tube. Moist rales are heard during both the inspiration and expiration, but since the air velocity is higher during inspiration, moist rales will be better heard at this respiratory phase.
Depending on the caliber of bronchi where rales are generated, they are classified as fine, medium and coarse (large) bubbling rales.
Depending on the character of the pathology in the lungs, moist rales are subdivided into consonating or crackling, and non-consonating or bubbling rales. Consonating moist rales are heard in the presence of liquid secretions in the bronchi surrounded by airless (consolidated) pulmonary tissue or in lung cavities with smooth walls surrounded by consolidated pulmonary tissue. The cavity itself acts as a resonator to intensify moist rales. Moist consonating rales are heard as if just outside the ear. Consonating rales in the lower portions of the lungs suggest inflammation of the pulmonary tissue surrounding the bronchi. Consonating rales heard in the subclavicular or subscapular regions indicate tuberculosis infiltration or cavern in the lung. Non-consonating rales are heard in inflammation of bronchial mucosa (bronchitis) or acute edema of the lung due to the failure of the left chambers of the heart. The sounds produced by collapsing air bubbles in the bronchi are dampened by the "air cushion" of the lungs as they are conducted to the chest surface.
Crepitation As distinct from rales, crepitation originates in the alveoli. Some authors erroneously classify these sounds as crepitant and subcrepitant rales. Crepitation is a slight crackling sound that can be imitated by rubbing a lock of hair. The main condition for the generation of crepitation is the accumulation of a small amount of liquid secretion in the alveoli. During expiration, the alveoli stick together, while during inspiration the alveolar walls are separated with difficulty and only at the end of the inspiratory movement. Crepitation is therefore only heard during the height of inspiration. In other words, crepitation is the sound produced by many alveoli during their simultaneous reinflation.
Crepitation is mainly heard in inflammation of the pulmonary tissue, e.g. at the first (initial) and third (final) stages of acute lobar pneumonia, when the alveoli contain small amounts of inflammatory exudate, in infiltrative pulmonary tuberculosis, lung infarction, and finally in congestions that develop due to insufficient contractile function of the left-ventricular myocardium or in marked stenosis of the left venous orifice of the heart. Crepitation can be heard in the inferolateral portions of the lungs of aged persons during first deep inspirations, especially so if the patient was in the recumbent position before auscultation. The same temporary crepitation can be heard in compressive atelectasis. During pneumonia, crepitation is heard over longer periods and disappears when a large amount of inflammatory secretion is accumulated in the alveoli or after its complete resolution. By its acoustic properties, crepitation can often resemble moist fine rales that are produced in fine bronchi or bronchioles filled with liquid secretion. Differentiation of moist rales from crepitation is of great diagnostic importance. Persistent crepitation may indicate pneumonia while fine nonconsonating rales suggest bronchitis. Differential-diagnostic signs of these rales and crepitation are as follows: moist fine rales are heard during both inspiration and expiration; they can be intensified or disappear after coughing, while crepitation can only be heard at the height of inspiration; it does not change after coughing.
Pleural friction sounds (murmur)
In physiological conditions, visceral and parietal layers of the pleura are constantly "lubricated" by pleural fluid and are therefore smooth. Their friction during breathing is noiseless. Various pathological conditions alter the physical properties of the pleural surfaces and their friction against one another becomes more intense to generate a peculiar adventitious noise, known as the pleural friction sound. Fibrin is deposited in inflamed pleura to make its surface rough; moreover, cicatrices, commissures, and bands are formed between pleural layers at the focus of inflammation. Tuberculosis and cancer are also responsible for the friction sounds. Pleural friction sounds are heard during both inspiration and expiration. The sounds are differentiated by intensity, or loudness, length, and site over which they are heard. During early dry pleurisy the sounds are soft and can be imitated by rubbing silk or fingers in the close vicinity of the ear. The character of pleural friction sound is altered during the active course of dry pleurisy. It can resemble crepitation or fine bubbling rales (sometimes the crackling of snow). In pleurisy with effusion, during the period of rapid resorption of exudate, the friction sound becomes coarser due to massive deposits on the pleural surfaces. This friction (to be more exact, vibrations of the chest) can be even identified by palpation of the chest. The time during which pleural friction sound can be heard varies with diseases. For example, in rheumatic pleurisy pleural friction is only heard 45 during a few hours; after a period of quiescence, it reappears. Pleural friction persists for a week and over in dry pleurisy of tuberculosis etiology and pleurisy with effusion at the stage of resorption.