
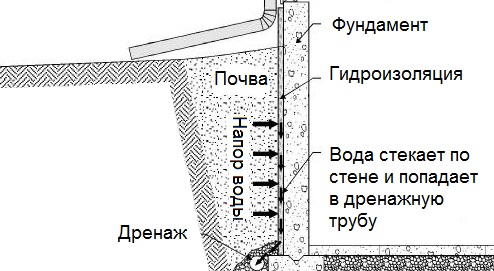
Общие условия выбора системы дренажа: Система дренажа выбирается в зависимости от характера защищаемого...
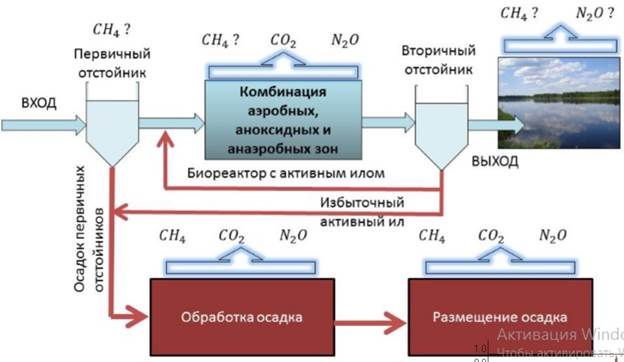
Эмиссия газов от очистных сооружений канализации: В последние годы внимание мирового сообщества сосредоточено на экологических проблемах...
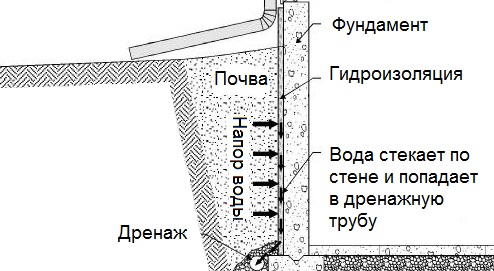
Общие условия выбора системы дренажа: Система дренажа выбирается в зависимости от характера защищаемого...
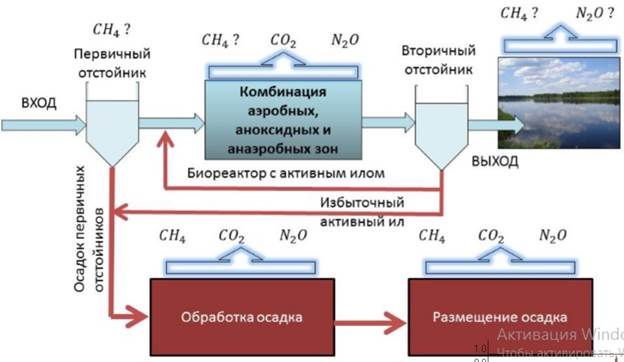
Эмиссия газов от очистных сооружений канализации: В последние годы внимание мирового сообщества сосредоточено на экологических проблемах...
Топ:
Отражение на счетах бухгалтерского учета процесса приобретения: Процесс заготовления представляет систему экономических событий, включающих приобретение организацией у поставщиков сырья...
Эволюция кровеносной системы позвоночных животных: Биологическая эволюция – необратимый процесс исторического развития живой природы...
Оценка эффективности инструментов коммуникационной политики: Внешние коммуникации - обмен информацией между организацией и её внешней средой...
Интересное:
Финансовый рынок и его значение в управлении денежными потоками на современном этапе: любому предприятию для расширения производства и увеличения прибыли нужны...
Отражение на счетах бухгалтерского учета процесса приобретения: Процесс заготовления представляет систему экономических событий, включающих приобретение организацией у поставщиков сырья...
Влияние предпринимательской среды на эффективное функционирование предприятия: Предпринимательская среда – это совокупность внешних и внутренних факторов, оказывающих влияние на функционирование фирмы...
Дисциплины:
|
из
5.00
|
Заказать работу |
|
|
|
|
| Cause | Frequent repeated bleeding from small vessels, usually mucous membranes (erosive esophagitis, gastroduodenitis, colon polyps, anal fissures, cervical erosion, etc.). |
| Questioning | Жалобы на слабость, утомляемость, головокружение, одышку и сердцебиение, звон в ушах, потемнение в глазах и мелькание «мушек» перед глазами, обмороки. Возможны жалобы на тошноту и тяжесть в желудке после еды, жжение языка и мышечную слабость. В анамнезе выявляется соответствующее заболевание. Complaints of weakness, fatigue, dizziness, breathlessness, and palpitations, ringing in the ears, darkening in the eyes and flickering of "flies" in front of the eyes, fainting. Possible complaints of nausea and heaviness in the stomach after eating, burning of the tongue and muscle weakness. A history of the appropriate disease. |
| General inspection | Pallor, dry hair and skin and peeling, atrophic glossitis, angular stomatitis, koilonychia. |
| Systems | RR and heart rate may be increased. Sound heart sounds, systolic murmur. |
| Lab data | Снижение концентрации эритроцитов, еще большее снижение гемоглобина, цветовой показатель около 0,5-0,6, микроцитоз, ретикулоцитоз или ретикулопения. Может наблюдаться анизоцитоз и пойкилоцитоз. Железо сыворотки и ферритин снижены. Reduced concentration of RBC, greater decrease of Hb, CI about 0.5-0.6, microcytosis, reticulocytosis/reticulopenia. Anisocytosis and poikilocytosis can be observed. Serum iron and ferritin are reduced. |
DICS (disseminated intravascular clotting syndrome)
| Cause | Severe trauma, hemorrhagic shock, extensive operations, placental abruption, burns, hemolytic transfusion reactions, prolonged cardiopulmonary bypass, sepsis, malignant hyperthermia, tumor products (tissue toxins), snake venom. |
| Questioning | Возможны жалобы на слабость, головокружение, одышку, на головную боль, боли в пояснице, жажду, тошноту и рвоту, уменьшение диуреза, кашель, боли в сердце. При желудочно-кишечных кровотечениях – мелена и пр. признаки. В анамнезе выявляется соответствующее заболевание. Complaints of weakness, dizziness, breathlessness, headache, lower back pain, thirst, nausea and vomiting, decreased urine output, cough, heart pain. In gastrointestinal bleeding - melena, etc. A history of the appropriate disease. |
| General inspection | It is characterized by lethargy, adynamia, in severe cases of impaired consciousness. The skin is pale/cyanotic, hemorrhagic rashes are possible, hemorrhage at the injection sites. Dyspnoea. In bleeding - the appropriate symptoms. Possible hypertonicity of muscles, psychosis. When combined with macrothrombosis, symptoms of arterial/venous thrombosis of large vessels (most often, venous thrombosis of lower extremities). |
| Systems | Signs of hemodynamic disorders up to shock, then cardiac output, CV, and CVP, systolic and pulse BP are reduced, in severe cases BP cannot be taken by the Korotkov’s method and no pulse on the peripheral arteries. RR and heart rate are significantly increased, the shock index is above 1. Signs of heart overload, hydrothorax, pulmonary edema, ascites, cardiac arrhythmias due to hyperkalemia are possible. In occurrence of bleeding - the appropriate symptoms. |
| Lab data | Hypercoagulation, followed by hypocoagulation. At this stage, a decrease of platelet count, an increase in bleeding time, clotting time, etc.; increase of thrombin time, prothrombin time, prothrombin index, INT, decrease of fibrinogen concentration, increase of D-dimers, thrombin-antithrombin complexes, plasmin-antiplasmin, etc., plasma fibrinolytic activity. Due to impaired tissue perfusion, a decrease in pH, oliguria/anuria, etc. |
Suppl. 6
|
|
EXAMINATION OF A PROCTOLOGICAL PATIENT
Directional survey.
A special survey reveals intestinal discomfort (constipation and flatulence). It is important to identify pains, their localization, origin, irradiation and connection with physical activity, emotional stress, food intake, an act of defecation. The time of onset and duration of pain should be clarified; if defecation disorder is accompanied by pain, the origin of this disorder should be identified.
Thus, acute “cutting”, “drilling” pain in the anus during defecation/immediately after it/ out of defecation (after a long walk/long sitting) is usually associated with the anal fissure, hemorrhoids, proctitis; while extending-pulsating pain in the perineum (outside of the anus) is typical for acute paraproctitis. Pain in the posterior semicircle of the anus, in the projection of the coccyx, aggravated by sitting, emotional stress, sometimes suddenly occurring at night, can be a symptom of coccyalgia. To relieve pain in the perineum (especially painful with an anal fissure), patients can set aside the leg, recarrying body weight to the other lower limb, or put the leg on a raised platform (because in this position the muscles of the pelvic floor relax and the intensity of pain decreases).
Abdominal pain, usually on the left, and especially in obese elderly patients, occurs with diverticular disease of colon, mainly in sigma diverticula. Chronic non-localized abdominal pain in combination with anemia and diarrhea are suspicious of diffuse inflammatory (ulcerative colitis) or tumor (polyposis) processes.
Anemia and prolonged defecation disorders as alternating constipation and diarrhea are among the first non-specific symptoms of colon cancer when the tumor is not yet palpated through the abdominal wall. In such cases, a colonoscopy is required.
The presence of tenesmus, false call for stools, feeling of a foreign body in rectum are typical both for hemorrhoids II-IV degrees, and for prolapse of rectum.
Acute abdominal pain and signs of intestinal obstruction testify, most often, to advanced tumor lesions of colon.
Another characteristic sign of proctological pathology is pathological discharge from the anus; most often it is mucus, pus and blood. It is necessary to clarify the number and type of pathological discharge, their association with defecation (before/during/after defecation). Having revealed obvious hematofecaly, it is necessary to find out the origin of bleeding (drips, sprays, flows in a stream, or remains as a strip on toilet paper). The last is more likely in acute anal fissure, especially in combination with severe pain in the anus during defecation. Scarlet blood as a trickle over feces, sometimes in significant quantities and without concomitant pains is a symptom of advanced hemorrhoids. Often, patients note the appearance of "piles", "tumors" from the anus, which is protruded internal hemorrhoids. Usually, in significant and frequent hemorrhoid bleeding, the piles cease to self-adjust into the lumen of rectum. Blood is “stale”, like “meat slops”, especially against the background of frequent defecation, tenesmus, can indicate both an exacerbation of ulcerative (granulomatous) colitis, and bleeding from a colon tumor. Oncopathology of colon, the discharge of blood "mixed with feces" and the fecal lump (in the form of a "pencil", "ribbon-like", etc.) are also characteristic. Syndrome of blood discharge from the anus without stool is very important, when you urge to defecate, a blood clot is discharged instead of stool. This is a formidable sign, often indicating the presence of a bleeding polyp/ulcerated tumor.
|
|
In the presence of pathological discharge, an immediate examination of the entire colon is required, especially if pathology is not detected with a rectal digital examination.
External inspection.
The first contact with a proctological patient should be as gentle as possible. On a gynecological chair (which is much more convenient for the doctor and more comfortable for the patient than the knee-elbow position), you must first examine the skin in the anus, make sure of no traces of scratching (anal itching), coarsening and thickening of the perianal skin or, conversely, its thinning; evaluate skin moisture (increased humidity often indirectly indicates sphincter weakness), identify areas of hyper- or depigmentation. Examine the area of the anus at rest and with a volitional contraction of the sphincter, check the anal reflex (contraction of the sphincter with dashed skin irritation of the perianal region). Pathological changes are visually determined: warts, condylomas, external hemorrhoids; postoperative scars (which can cause both a gaping of the anus due to cicatricial deformity, and its severe stricture), external openings of pararectal/sacrococcygeal fistulas. The anus area is examined both at rest and with a sphincter volitional contraction, the severity of the anal reflex is checked.
With careful pushing the buttocks in patients with complaints of acute pain, you can see ad oculus the wall of the anal canal (most often on the back), longitudinal crack-ulcer, clotted hemorrhoids, a polyp falling out of the anus on a long crux; a point hole (sometimes several holes located in a row one after another) along the midline, immediately above the posterior semicircle of the anus, with hair sticking out of these holes (epithelial coccygeal duct); painless subcutaneous masses (dermoid cysts).
After this local examination, palpation of the entire abdomen, the edges of the liver and inguinal lymph nodes is necessary.
Digital rectal examination.
This the most important and mandatory diagnostic manipulation is still the main for determining proctological pathology. Rectal examination is primary, it must be performed before any instrumental manipulations, such as anoscopy, recto- or colonoscopy. A digital examination of rectum is usually performed without exacerbation of a disease (hemorrhoids, anal fissure), and then it is only unpleasant for the patient, while forcing the finger into the inflamed, spasmodic anal canal causes sharp pain, which complicates further communication with a patient. Usually, according to complaints and external examination, you can understand that a digital examination will be painful, and it is better to postpone it until the acute phenomena will be arrested. In case of acute pain and diagnostic difficulties, a digital rectal examination can be performed under local anesthesia.
|
|
Preparing patient with enemas for an initial examination is not required. If a rectal digital examination is performed in the first half of the day, then the rectal ampoule should normally be empty - this is an important sign of a full morning defecation. The careful introduction of a well-oiled index finger into the anus usually gives the doctor understanding of the function of the rectum obturator mechanism. The finger is inserted for the entire length along the posterior surface of the anal canal and then, conducting it along the circumference of the walls, examining them usually to a depth of 8-10 cm, and using a special technique, straining the patient in a squatting position, determine the condition of the intestine up to 11-12 cm from the outer edge of the anus. If previously, during an external examination, a painful area is found on the back wall of the anal canal, then the finger is inserted along the opposite wall.
First, determine the state of the walls of the anal canal. Normally, they are smooth, in the the lower ampoule area - as ribbed due to the presence of alternating longitudinal grooves and elevations (anal crypts and columns). The lower parts of crypts are felt like pits, bounded below by peculiar dense flaps - "pockets" that create a circular dental line. Individual dense dents (papillae) are often misinterpreted as “anal polyps”. Small stool particles can stagnate in the “pockets” of anal crypts, which often leads to local inflammation (cryptitis) or to more common inflammation of the rectum and sigmoid colon (distal proctitis, proctosigmoiditis). In inflammation of crypts, painful micro-abscesses are determined, they may serve as sources of acute and chronic paraproctitis or trophic ulcers of the anal canal (chronic anal fissure). All these normal anatomical structures and pathological changes should be identified by digital rectal examination.
In addition, large dense polyps and malignant tumors are determined with a finger. Colorectal cancer in all cases is detected precisely with a digital examination. The size, consistency, tuberosity, ulceration, hemorrhage of the tumor, its mobility from the mucosa and the degree of its growth into the deep layers of the rectum - all these most important parameters are initially determined by the finger. If a finger examination determines the lower edge of a dense intraluminal mass, then you should additionally try to feel the tumor in the patient’s squatting position with a straining.
In pains in the anus with radiation to the sacrum and tailbone, as well as for independent pain in the sacrococcygeal region, a two-finger study is used: the index finger is inserted into the anus, and the coccyx and sacrococcygeal joint are felt with the thumb of the same hand. In this case, mobility (balloting) of the coccyx tip is sometimes determined, which may indicate old fracture; in such cases, radiography of the sacrum and tailbone in two projections is required. Also, with a finger study, pain and tension of the anal levator muscles are determined, which helps to clarify the origin of the anal-coccygeal pain.
In women with gynecological complaints, a bimanual recto-vaginal examination is necessary to identify possible pathology of the recto-vaginal septum (scars, cysts, thinning and defects with the formation of rectocele, fistulas, etc.), especially in multiparous patients. In urological complaints, especially in elderly patients, it is necessary to palpate the prostate gland and consult a patient with a urologist. It should be emphasized that in many cases a common examination of a proctologist, urologist (sometimes andrologist) and/or gynecologist is necessary.
|
|
Only after completing all the described procedures and determining the tone and volitional contraction of the anus sphincter, finding out the absence of painful spasm of the anal muscles, strictures and other obstacles for instrumental examination, you can proceed to it. Anoscopy with an ordinary rectal mirror without anesthesia, as well as a sigmoidoscopy with a rigid apparatus without appropriate preparation, are extremely uncomfortable, and often very painful and not very informative. Often, limited only by rectoscopy (examination of 18-20 cm), the doctor skips the pathology of the right colon, especially the asymptomatic adenomatous polyps (obligate precancer), found with total flexible colonoscopy.
Anoscopy
Examination with a conventional anoscope, and even with a branched rectal mirror, due to its low informative; it is preferable to study with a modern anoscope with central illumination/a sigmoid (sigmoid) scope. The best option is fibrocolonoscopy. However, in anoscopy, it is possible to see enlarged internal hemorrhoids (sometimes, due to their elasticity, emptying, poorly defined by digital examination), acute anal fissure, chronic anal fissure, polyp or malignant tumor of the anal canal and lower ampoule area. Anoscopy well complements the digital rectal examination, and allows to identify the localization of the inner holes of the pararectal fistula (in most cases, opens in the projection of the posterior or anterior central crypt), as well as visually assess the degree of scar changes, the length of the stricture of the anal canal. Due to the limited length of the apparatus, the method does not allow to verify fully the pathology from the middle part of the rectal ampoule, and even more its upper ampullar part. Nevertheless, based on the fact that 80% of proctologic pathology mainly affects the rectum and distal third of the sigmoid colon single and multiple polyps, most colorectal cancers, ulcerative colitis, for the purpose of mass primary screening, rectoromanoscopy (RRS) (sigmoidoscopy) is still relevant.
RRS
Until recently, the procedure for examining the rectum and distal third of the sigmoid colon with a hard metal rectoscope of a sufficiently large diameter is uncomfortable for patients, and if possible, it should be preferred to flexible sigmoidoscopy, in which instead of 25-30 cm it is really possible to examine 55-60 cm of the distal colon. If it is necessary to perform RRS with a rigid instrument, the patient is examined in the knee-shoulder position, and in a patient’s severe condition - on the left side with the knees bent to the stomach. Initially, a rectoscope tube with an obturator inserted into it, richly lubricated with an indifferent oil, is introduced by rotational movements for a depth of 5 cm in order to only pass the anal canal. At the same time, they ask the patient to relax and take a deep breath. After passing the sphincter, the obturator is removed, the eyepiece is connected and further advancements are carried out only under the control of vision; constantly inflated air, conduct the tube forward, constantly focusing on the lumen of the intestine, following its bends and gently pushing the folds of the mucous membrane with the end of the tube. In no case, during the procedure, you can’t make sharp frictional movements with the end of the tube to avoid damage to the wall! During the introduction of the tube, a detailed examination is not carried out, but only try to insert the tube to the end as less painfully as possible. If pain occurs (it’s nor normal), the procedure should be stopped immediately. Pain in RRS is an important diagnostic sign, indicating either an anatomical variant of the location of the colon (kink) or extra-intestinal constriction (more often in women after inflammatory diseases of the internal genitals/after gynecological surgery), as well as extraintestinal mass (abscess, infiltrate, tumor).
A detailed thorough examination of the distal third of the sigmoid and rectum is performed as the device is removed. The extraction of the tube should also be smooth, reverse traction must be combined with methodical rotational movements in a spiral from depth to outside, during which all visible changes in the intestinal wall are recorded; it is necessary to try not to miss the pathology located behind the mucosa folds. The degree of intestine preparation for the study is evaluated. So, if the preparation is poor, it is impossible to adequately verify any changes of the mucosa, it is likely to miss small polyps and even endophytic cancer.
|
|
It is important to note whether the lumen of the intestine is free, how much the capacity of the ampoule is changed (normal, narrowed, or expanded). It is also noted that there is no pressure on the intestine from the outside (usually due to adhesions and pelvis tumors, pregnant uterus), which is usually reflected as deformation and narrowing of the lumen of the ampoule or rectosigmoid section, and complicates further research. The elasticity (atony, rigidity) of the mucosa folds, their height is assessed. If free mucus is found in the lumen, as well as feces, they describe the approximate amount of contents, color, consistency, pathological impurities.
In satisfactory preparation of the intestine, in addition to small pathological neoplasms in the form of forming polyps (size from 0.2-0.3 cm in diameter), it is possible to see the mouth of the sigmoid colon diverticulum, various changes in the mucous vessels. In this case, it is necessary to characterize them qualitatively (injection, or blurry vascular pattern, its impoverishment, pallor or severe hyperemia), to note the degree and prevalence of edema, inflammation. One should evaluate its contact vulnerability and profuse scraping with suspected proctosigmoiditis. Petechial hemorrhages, as well as ulcerative erosive lesions with fibrin overlay, often in combination with inflammatory pseudo-polyps, are typical for ulcerative colitis, and deep longitudinal ulcers-cracks in alternation with islets of granulations (“cobblestone pavement”, colonic Crohn's disease). More rare diagnostic findings include hemangiomas, benign strictures of various origins, submucosal neoplasms.
If a malignant tumor of the rectum is detected during RRS, its size, length along the circumference of the intestine (and if the apparatus succeeds in reaching the upper pole of the tumor, then along the length of the intestine), as well as the surface of the tumor, its consistency, type of growth (ex/endophytic), the vulnerability, the mobility of the neoplasm relative to the underlying layers of the intestinal wall, the degree of possible ingrowth into the underlying tissues (should be further verified and documented by endorectal ultrasound examination and CT/MRI).
In this case, it is possible to take scrapes (fingerprints) from suspicious sites for cytological examination or biopsy of tumor using a conchotome for a histopathological examination.
If a narrowing of the lumen is detected, they sometimes use a pediatric proctoscope (with a reduced diameter of the tube), but you can’t try to go above the obstacle at any cost, this can lead to iatrogenic damage to the colon. In this case, it is better to prefer flexible sigmoidoscopy or FCS.
О bligatory FCS
Due to the sharply increased incidence and “rejuvenation” of colorectal cancer, the idea of mandatory primary preventive colonoscopy for all people over 50 years of age is discussed. High risk groups for colon tumors include, first of all, patients with unclear abdominal pain and "unmotivated" stool disorders, regardless of the presence/absence of occult blood in feces.
Last decades, such mandatory and previously performed in all cases diagnostic procedure, as rigid sigmoidoscopy (RRS), has been successfully replaced by flexible colonoscopy. In any signs of intestinal discomfort, primary FCS is necessary. This is the only way to detect early forms of colon cancer, the incidence of which is increasing worldwide.
The main indications for FCS: the presence of multiple (2 or more) polyps in the rectum, detected by RRS; control after removal of polyps and after operations for colon cancer; rectal bleeding; changes in bowel function; polyps and colon cancer in relatives and some others.
It is highly desirable that the doctor conducting FCS is not only an endoscopist, but also a surgeon, as often diagnostic endoscopy in becomes curative. So, when polyp on the crux or with a diameter above 5 mm are detected, its electroexcision is performed. It should also be noted that asymptomatic polyps and even early forms of cancer can be found in the right parts of the colon, inaccessible for RRS/sigmoidoscopy, no less than in its left flank that’s especially typical for patients with identified distal polyps.
A total FCS with examination of the terminal ileum should be peformed, i.e. with penetration behind the ileocaecal valve. This gives an idea of the function of the ileocecal valve, the state of the mucous membrane of the terminal part of the ileum, where inflammation is often localized in Crohn's disease (terminal ileitis).
Irrigoscopy (graphy)
Irrigoscopy (X-ray examination of the colon using a barium enema) should be prescribed only if total colonoscopy fails, in a colon stricture, or any other abnormality, as well as the inability to perform FCC for any reason. In irrigoscopy (graphy), besides a significant dose of radiation for the patient and the doctor, it is impossible to identify and interpret small (below 1 cm in diameter) polyps those are not always harmless. Irrigography is uninformative about the rectum and distal third of the sigmoid colon, i.e. before irrigoscopy, RRS is needed.
Computer colonography
A relatively new method - virtual colonoscopy/computed tomographic colonography - is an expensive method that can be used for special indications. So, it allows you to get a three-dimensional image of both the external contours and the lumen of the colon in 2-3 projections, which makes it possible to assess the condition of the intestinal wall (thickening), determine near rectal enlarged lymph nodes, see the smallest polyps, etc.
References
|
|
|

Таксономические единицы (категории) растений: Каждая система классификации состоит из определённых соподчиненных друг другу...
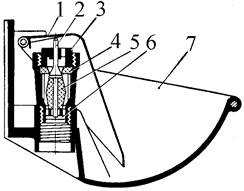
Индивидуальные и групповые автопоилки: для животных. Схемы и конструкции...
Механическое удерживание земляных масс: Механическое удерживание земляных масс на склоне обеспечивают контрфорсными сооружениями различных конструкций...
Археология об основании Рима: Новые раскопки проясняют и такой острый дискуссионный вопрос, как дата самого возникновения Рима...
© cyberpedia.su 2017-2024 - Не является автором материалов. Исключительное право сохранено за автором текста.
Если вы не хотите, чтобы данный материал был у нас на сайте, перейдите по ссылке: Нарушение авторских прав. Мы поможем в написании вашей работы!