2.1. General inspection.
Inspection is the first objective physical method of clinical examination, carried out simultaneously with questioning, palpation, percussion and auscultation. During a general examination, the state of consciousness, facial expression, position, gait and posture, general appearance, physique, condition of skin and visible mucous membranes, hair and nails, subcutaneous fat, musculoskeletal system are determined. First, a general inspection is made, and after a local one. Local examination involves a sequential detailed examination of parts of the body according to a certain pattern: limbs, head, face, neck, oral cavity, chest, abdomen.
During inspection, the following conditions must be observed:
a) Inspection is preferably carried out in natural daylight, as artificial light sources can distort the color of skin, the configuration of body parts;
b) Patient’s illumination should be direct and lateral. If direct, the light source should be located opposite the patient, if lateral - on the right/left from him/her. The doctor is always facing the patient. With direct illumination, the contours of body parts and its color are determined, in lateral illumination, motility of internal organs (breathing excursion, abdominal wall, visible intestinal motility, epigastric pulsation, etc.) are well defined;
c) Before the examination, the patient should be naked to the waist, while examining the abdomen - from the middle of the chest to the middle of the thighs. The body and chest are best examined in the vertical position of the examinee, the abdomen - in vertical and horizontal positions;
d) First, patient’s general condition is assessed, it can be satisfactory, moderate, severe, extremely severe, terminal. The severity of the condition may be due to the severity of the pathological process, the degree of functional disorders of organs and systems, as well as the likelihood of complications of the disease.
The patient’s consciousness at the time of examination can be clear (the patient is fully oriented in time and space, his personality, coherent thinking, memory for current and previous events of the disease is preserved), excited (for example, caused by severe intoxication with pancreatic necrosis, up to severe hallucinations), confused (stupor, sopor, coma).
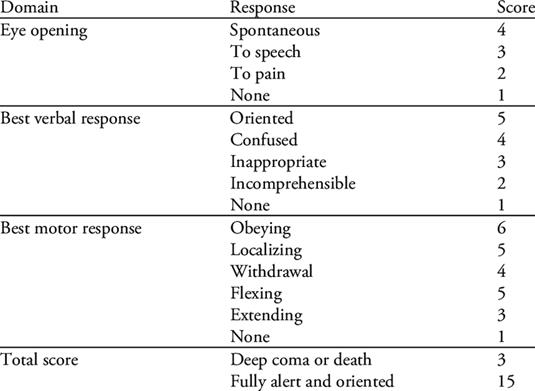
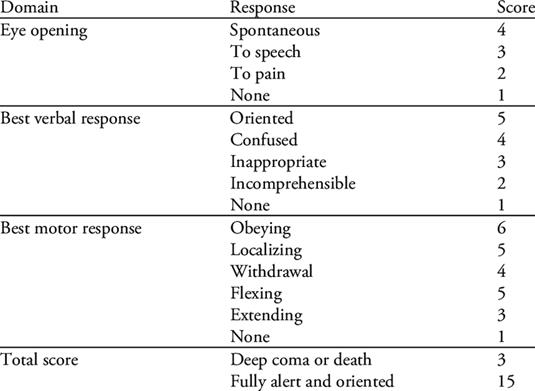
Stupor - a patient is disoriented in the surrounding space, inhibited, adynamic, fuzzy answers to questions, reflexes are prersent; sopor - a state similar to a dream, from which the patient can be withdrawn with a strong irritant (pain), can answer monosyllables with a delay; coma is characterized by a complete loss of consciousness, absence of reflexes, involuntary urination and defecation. At the stage of examination, when it is still impossible to make a comprehensive conclusion, the Glasgow scale is used to assess the state of consciousness (spl. 1).
Patient’s position. If the patient moves freely and changes position arbitrarily without any difficulty, then he/she is active. If it is impossible for the patient to arbitrarily change his position, it is called passive and, if the patient purposefully takes a certain position in order to facilitate painful manifestations, it is forced. Lying, sitting and standing forced patient’s position may be observed. The supine position can be on the back, on the abdomen or on the side. Forced position on the back is observed in the presence of severe abdominal pain (perforated ulcer, appendicitis, peritonitis, etc.). Forced position on the abdomen is often noted in spinal tuberculosis. On the side patients most often lie with unilateral hemothorax, pneumothorax, fractured ribs, lung abscess. The forced sitting position (orthopnea) occurs mainly in shortage of breath in patients with cardiac/respiratory failure (pulmonary edema, pneumothorax, mediastinal emphysema, etc.). The forced standing position is observed in an attack of intermittent claudication (a symptom of "showcase").
Body type. The following constitutional types are observed: hypersthenic (medium or short stature, increased fatness, relatively short arms and legs, a rounded head, a short neck, a wide chest, a protruding stomach, epigastric angle> 90°), asthenic (growth above average, thin, elongated neck and narrow chest, epigastric angle <90°), normosthenic (occupies an intermediate position).
Anthropometric data: height, body weight, posture (straight, stooped); gait (fast, slow, atactic, spastic, paretic, etc.).
The skin and visible mucous membranes. On examination, pay attention to the color (pale pink, pale, hyperemic, cyanotic, icteric, bronze, gray, earthy, etc.), rash, hemorrhage, peeling, scarring (if available, indicate localization, dimensions, color, direction)
Skin moisture (normal, enhanced, dry).
Skin elasticity (skin is elastic/flabby, skin turgor is retained/reduced).
Subcutaneous fatty tissue – students must assess the degree of development, the location of the largest deposits, the thickness of the skin folds on the shoulder, pain in palpation, the presence of focal seals, crepitation (subcutaneous emphysema).
Swelling. If available, indicate localization (face, eyelids, limbs, lower back, general); severity; consistency (dense, soft, pasty); symmetry (symmetrical edema of extremities, face, abdominal wall may indicate at renal/heart failure, asymmetric edema of extremities indicate at local blood flow disorders); day dynamics (appear or intensify in the evening, after physical exertion, prolonged orthostatic position, or constant during the day).
Body temperature: low (below 36°C), normal (36-37°C), subfebrile (up to 38°C), febrile (up to 39°C), high (over 39°C), excessively high (over 40°C), hyperpyretic (above 41-42°C).
Lymph nodes. Describe the main groups of subcutaneous lymph nodes (submandibular, cervical, occipital, supraclavicular and subclavian, axillary, inguinal). Indicate the groups of enlarged lymph nodes, their sizes, shape, consistency, pain, mobility/adhesion to each other and to surrounding tissues, skin changes above them (redness, blueness, ulceration). Changes in the lymph nodes occur as a reaction to the inflammatory process (inguinal lymphadenitis with erysipelas of the lower limb), or as metastasis of the anal cancer, metastasis to the axillary collectors for breast cancer, etc. A common enlargement of lymph nodes indicates a systemic lesion of lymphoid tissue (leukemia, lymphogranulomatosis). In tuberculosis, the lymph nodes are enlarged, “fuse” into packets, suppurate with the formation of fistulas.
Locomotor system. Muscles: the degree of development (satisfactory, weak, atrophy), tonus (normal, increased, decreased), cramps (in the presence of seizures, tonic/clonic). Bones: curvature of the spine (scoliosis, kyphoscoliosis), pain in palpation, pathological mobility (in the presence of pathology, indicate localization). Joints: deformation, range of mobility (active, passive), pain in movement, skin discoloration and temperature above the joints, crunching and fluctuation. In surgical practice, joint pathology is observed in acute bacterial arthritis, bursitis, tuberculosis, intra-articular localization of osteomyelitis, metastatic bone lesions.
2.2. Respiratory system
Nose: nose shape; breathing through the nose (free/difficult). Nasal discharge, its nature and quantity. Nosebleeds.
Pharynx: deformation and swelling in the pharynx.
Voice (loud/quiet, clear/husky, lack of voice - aphonia).
Chest. When examining the chest, determine its shape (normosthenic, asthenic, hypersthenic); the shape of the supra- and subclavian fossae (filled, protruding, retracted); width of the intercostal spaces (protruding, retracted); the shape of epigastric angle (obtuse, straight or sharp); position of scapulae and clavicles (tightness, deformation); symmetry of both halves of the chest (enlargement/diminution of one of the halves, retraction/protrusion); type of breathing (thoracic, abdominal, mixed); symmetry of the respiratory movements (the presence of delay on one of the halves); participation of auxiliary muscles in the breathing; the incidence of respiratory movements per a minute; depth of breath (superficial/deep); breathing rhythm (rhythmic/arrhythmic); the ratio of the length of the inhalation and exhalation (expiratory, inspiratory or mixed breathlessness).
In palpation, determine the presence of painful areas and their localization; chest elasticity; voice trembling on symmetrical sections of the chest (same, weakened or strengthened, indicate localization according to anatomical landmarks).
In percussion, conduct comparative and topographic examination of both lungs (sound: clear pulmonary, dull, box-shaped, tympanic), determine the borders via vertical lines and an excursion of their lower edges.
In auscultation, describe respiratory murmurs: vesicular (weakened/intensified) and physiological bronchial, as well as pathological types of breathing and noises (amphoric breathing or lack of breathing noise, rales, crepitations, pleural friction noise) on symmetrical parts of the chest with exact localization according to intercostal space and topographic lines.
2.3. Circulatory system
a) examination of cardiac area.
When examining, pay attention to the condition of the external jugular veins and carotid arteries (visible pulsation, dilation, etc.); protrusion in the cardiac area (gibbus cordis); visible pulsations (apical/cardiac beat, epigastric pulsation, pulsation in the jugular fossa, atypical pulsation in the cardiac area). If available, indicate localization, power, relation to the phases of cardiac activity. Percussion determines the relative and absolute borders of cardiac dullness, the configuration of heart (normal, mitral, aortic, mixed). Auscultation characterizes the rhythm of heart contractions (regular/arrhythmic), heart rate, the presence of pericardial friction noise.
b) The examination of arteries.
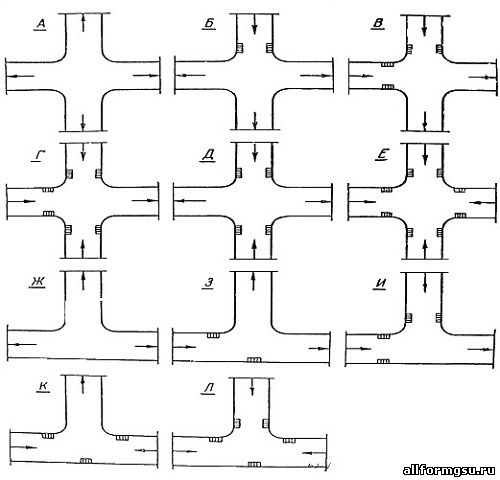
Inspection and palpation. When examining peripheral vessels (first arteries, and then veins), follow the general sequence of actions (examination, palpation, auscultation). In examination, pay attention to the position of the limbs, skin color, hyperpigmentation, the presence of trophic skin disorders (dryness, peeling, ulcers, hairline changes, swelling of extremities, fungal infection of the nails). Palpation is carried out on symmetrical vessels on the right and left, and the results are to be compared with each other.
Palpation of the following arteries is performed:
§ superficial temporal artery palpated anterior to the auricle floor (tragus)
§ carotid - inside from the sternocleidomastoid muscle at the level of thyroid cartilage;
§ axillary artery - at the bottom of the armpit, asking the patient to raise a straightened arm, and the artery is pressed against the head of humerus;
§ brachial artery - in sulcus bicipitalis medialis;
§ femoral artery - under the inguinal ligament, in the position of the patient lying with the thigh slightly turned outwards;
§ popliteal artery - in the popliteal fossa in the lying patient’s position with a bent leg in the knee joint;
§ posterior tibial artery - in the condyle groove, slightly behind and below the medial ankle;
§ dorsal artery of the foot - in the first intertarseal space.
Auscultation. We perform auscultation of abdominal aorta (along the midline in the umbilical area), other arteries: carotid (inside the sternocleidomastoid muscle at the level of the upper edge of the thyroid cartilage), subclavian (under the clavicle in the deltoid-thoracic triangle), shoulder (in the elbow bend at outstretched arm) and femoral (under the inguinal ligament). During auscultation of arteries, conducted noises can be heard (on the carotid and subclavian arteries in stenosis of aortic valve), in dilation of artery (aneurysm) or its narrowing (if compressed from the outside).
Arterial pulse. Comparison of the pulse wave in both radial arteries: frequency, rhythm, deficiency, arrhythmias, filling, tension, speed. Blood pressure (BP). Measurement of systolic and diastolic blood pressure by Korotkov’s method on the right and left brachial arteries (in mmHg).
b) Symptoms and tests in the examination of peripheral arteries.
Oppel’s test. Sign of peripheral arterial circulatory failure: the patient, lying on the back, raises lower limbs, bent in the knee joints under 45°, and holds them in this position for 1 min. In case of insufficiency of peripheral arterial circulation in the sole area on the affected side, pallor occurs, which is normally absent.
Leignel - Lawastine test Sign of thrombobliterative artery disease: when pressing on the sole/palmar surface of the distal phalanges of the first toe, a white spot appears at the pressure site, which normally holds for 2-4 seconds. Prolongation of blanching time above 4 sec indicates a violation of blood circulation.
Samuels Symptom. Sign of circulatory disturbance in the extremities: a patient in a supine position is offered to raise both straightened legs and make quick flexion and extension movements in the ankle joints. In case of circulatory disturbance, after 1-2 minutes blanching of the feet occurs. To study the vessels of the upper extremities, the patient raises his hands up and clenches his fists several times. If blood circulation is disturbed, the fingers turn pale.
c) The examination of veins.
Inspection and palpation of the external jugular veins: dilation, pulsation. The presence, localization and severity of the dilation of the veins on the chest, abdominal wall (porto-caval anastomoses) and limbs. Infiltration, presence of skin changes and palpable of soreness along the veins. Palpation of superficial veins of lower extremities (the presence of varices, pain at the points of projection of perforating veins).
Symptoms and tests in the study of peripheral veins.
Hackenbruch - Sicard Symptom. A sign of valve insufficiency in sapheno-femoral junction: a doctor puts a hand to the thigh at the place below inguinal ligament and offers the patient to cough. In this case, a push (a positive symptom) is felt, indicating a failure of the vein valves. When coughing as a result of contraction of the diaphragm, a back wave of venous blood from the inferior vena cava occurs. It is transmitted through the common and external iliac vein into the femoral and large saphenous veins.
Sheinis test. It serves to determine the insufficiency of the valves of the communicative veins. In the patient’s supine position, the tested limb is raised vertically and three tourniquets are applied, compressing only the saphenous veins - under the oval fossa, in the middle third of the thigh and under the knee. After this, the patient stands up. The appearance of dilated veins in any area indicates the insufficiency of valves of communicative veins within this segment.
Brodie — Trendelenburg Test. Indicates the failure of the valves of superficial veins: for a patient with varicose veins in the supine position, they raise the leg, while the visible veins collapse. The saphenofemoral junction is pressed with a finger/a soft rubber tourniquet that is applied to the upper third of the thigh. When moving to a vertical position, the saphenous veins of 15-30 sec remain collapsed - and gradually are filled with blood from the periphery. If the tourniquet is removed, the varicose veins of the thigh and lower limb are filled in a few seconds with a top back blood flow, which indicates the usefulness of the valves of the connecting veins and the insufficiency of the valves of the great saphenous vein - the test is positive.
Delbet-Perthes test, march test. A sign of obstruction of the deep veins of a lower extremity: a patient in an upright position, an elastic tourniquet is applied in the upper third of the thigh (the tension of the tourniquet is only to compress the saphenous veins), and a patient is offered to walk around the room. If, after this, the saphenous veins are emptied and subside, consider that the deep veins are passable; if they do not subside, then deep vein patency is impaired.
2.4. Digestive system.
Oral cavity: tongue (color, humidity, condition of the papillary layer, the presence of plaque, cracks, ulcers); condition of teeth; gums, soft and hard palate (coloration, plaque, hemorrhage, ulceration); the presence of odor from the mouth (smell of acetone, fresh hay, “putrid” odor, etc.).
Abdomen: Inspection of the abdomen is carried out both in horizontal and vertical position of the patient, which allows better identification of existing changes. Pay attention to the following parameters:
a) Shape. In exhaustion, the abdomen becomes retracted, in thickening the subcutaneous fat layer, flatulence, significant ascites, the abdomen is noticeably enlarged. In persons with weak abdominal muscles, especially with splanchnoptosis the abdomen becomes saggy. In the accumulation of a small amount of fluid in the abdominal cavity, it is located mainly in the side sections, as a result of which the abdomen becomes flattened. Symmetry (the shape of the abdomen changes in the presence of large hernias, uneven bloating of the intestine with intestinal obstruction, deforming scars of abdominal wall, large cysts and tumors of the abdominal cavity, retroperitoneal space and pelvis);
b) Participation in breathing (in acute inflammatory diseases/injuries, the sections of the anterior abdominal wall may not equally participate in breathing due to local muscle tension);
c) Visible peristalsis of stomach and intestine (can be observed in cachectic patients, pyloric stenosis or acute intestinal obstruction).
d) The presence, localization and severity of venous collaterals on the abdominal wall (indicates a violation of venous outflow in the portal and inferior vena cava system).
Palpation of abdomen. It is carried out methodically (by Obraztsov-Strazhesko). In superficial palpation, special attention is paid to localization of painful areas; muscle tension of abdominal wall; diastasis of rectus abdominis muscles, the presence of protrusions wall during breathing and straining in typical "anatomically weak places"; peritoneal symptoms (Shchyotkin-Blyumberg, Mendel symptom, etc.); presence of superficial tumor masses.
In deep palpation, the characteristics of all parts of intestine (pain, size, shape, surface, mobility and rumbling), pancreas, lower edge of liver (indicating shape, density, surface, soreness) and gallbladder are indicated. In the presence of tumor mass/infiltrates, their sizes, consistency, soreness, mobility, localization and possible connection with abdominal organ are described.
In percussion, the nature of percussion sound is established, the presence of signs of free/localized fluid in the abdominal cavity, the sizes of liver (by Kurlov) and spleen are determined.
Auscultation is necessary to assess peristaltic intestinal sounds heard (weakened, strengthened, not changed, absent), peritoneal friction noise.
Manual examination of rectum.
A rectal examination is performed for all patients above 50 years old. The examination assesses the condition of the perineal area and anal ring (presence of cracks, ulcers, infiltrates, hyperemia, hemorrhoids, fistulas), sphincter tonus, rectal wall changes (elasticity, smoothness, pain, infiltration, narrowing), adjacent organs (prostate and seminal vesicles in men and internal genital organs in women, coccyx, sacrum, neck of the bladder), condition of the peritoneal pelvic fold (pain, “overhanging”), contents of rectum lumen (blood, pus, mucus remaining on the glove, consistency of feces).
2.5. Urinary system.
Inspection of the lumbar region (hyperemia of skin, asymmetry of the areas). Inspection of the suprapubic area (contouring of overfilled bladder).
Palpation foresees examination of kidneys in the supine and standing position (if palpable one should to determine pain, consistency, size, shape, mobility, surface nature, symptom of balloting); urinary bladder (level of the bottom and its soreness); characteristic points of pain (in the corner between the XII rib and spine; at the outer edge of rectus abdominis muscle at the navel level; at the intersection of the line connecting anterior superior iliac spines with a vertical line passing through the pubic tubercles).
Determination of beating symptom. The symptom of beating is usually determined in patient’s standing/sitting position, but if necessary, it can also be checked in patient’s supine position, putting the hands under the lumbar area and providing beatss with them. Depending whether a patient has pain at the time and how intense it is, the symptom is regarded as negative, weakly positive, positive and sharply positive. A positive symptom is noted in urolithiasis (especially at time of renal colic), acute pyelonephritis, paranephritis, etc.
The definition of the upper border of the bladder is carried out by percussion, conducting it from the navel to pubic symphysis bottom along the midline.
2.6. Examination of endocrine system.
includes examination of the neck, thyroid palpation and determination of special eye symptoms, indicating thyrotoxicosis.
When examining the front surface of the neck, you can find thyroid enlargement (goiter), associated with change the neck shape. In such cases, pay attention to the symmetry of the neck.
Palpation of thyroid determines its size (indicate the degree of enlargement of the gland according to WHO), surface (smooth or tuberous), consistency (elastic, dense, stony), the presence of nodes, adhesion to surrounding tissues, mobility in swallowing, soreness.
In patients with toxic goiter, eye symptoms are detected: Dalrymple’s (expansion of the palpebral distance with the presence of sclera strip above the iris), Stellwag’s (rare blinking), Moebius’s (weak convergence), Kocher’s (the appearance of the same strip of sclera between the upper eyelid and iris when the eyeball moves upward, i.e. the lag of the eyeball from the upper eyelid), Rosenbach's sign (tremor of eyelids), and Jelink's sign (hyperpigmentation of the eyelid).
2.7. Examination of the neuropsychic sphere.
It is necessary to evaluate whether the patient is oriented correctly in space, time and proper person. To do this, ask some questions: “Where are you now?”, “What day of the week, month, year is it today?”, “Please indicate your last name, first name, middle name”, etc. At the same time, note, please, whether the patient is willingly contacting a doctor.
3. DESCRIPTION OF A SITE OF A DISEASE (STATUS LOCALIS)
The correct preparation of this chapter in surgical practice is of great importance, since often the local manifestation is the main disease (tumor, wound, fracture, dislocation, osteomyelitis, bone tuberculosis, burns, etc.), and correct diagnosis and treatment effectiveness depends on the correct interpretation of clinical data.
When describing the local status, it is necessary to follow a certain plan:
§ First, the examination of the lesion area is described, then the data obtained by palpation of this area is described;
§ If the lesion is an independent local disease, then the examination first describes the lesion, and then the surrounding tissue;
§ If the visible focus is a manifestation of a general disease (gangrene of a limb segment in obliterating atherosclerosis, trophic ulcers in chronic venous insufficiency), then the entire anatomical region is described first: the condition of skin, soft tissues of the limb, and then the lesion itself;
§ Status is described in coherent text, without dividing into subparagraphs (examination, palpation, etc.), changes that are absent in a patient are not described.
Inspection
§ Indicate a clear anatomical location of the lesion;
§ Make a visual comparison (if possible) of the changed area with the symmetric unchanged one;
§ Skin: color (pale pink, pale, cyanotic, icteric, hyperemia); skin rash: form of rash (roseola, papules, pustules, vesicles, erythema, spots, bullae), localization of rash (single or multiple); scars (localization, color, size); trophic changes of skin (peeling, thinning, hair reduction, areas of hyper- and depigmentation); the borders of the lesion (clear, fuzzy); at what level to healthy skin is the altered area of skin (rising, at one level, retracted); contour of the altered area (smooth, uneven, specific shape (“flames”, “geographical map”));
§ Subcutaneous fat (thickness defines with a skin fold, the presence of visible volume formations);
§ Muscles (atrophy, hypertrophy);
§ Bones (visible deformations);
§ If there is a defect of skin (scarifications, wounds, trophic ulcers, necrosis, fistulas), describe it (if there are several defects, each should be described separately) according to the following plan: dimensions (length, width, depth); direction via the longitudinal axis of the anatomical area (longitudinal, oblique, transverse); edges (smooth, uneven, eroded, crushed, callous); bottom (what tissues make the bottom of the wound); discharge: character (serous, hemorrhagic, purulent, putrefactive, mucous), consistency, smell, presence of impurities (clots, detritus), quantity.
Palpation:
§ soreness;
§ local hyperthermia;
§ Infiltration (localization, sizes);
§ volumetric masses (tumor, hematoma): density, consistency, displacement, fluctuation, and softening;
§ presence of edema, its severity;
§ regional lymph nodes (groups of lymph nodes located in the closeness of the lesion): sizes, adhesion to surrounding tissues, pain in palpation, consistency, skin color above the lymph nodes.
Assessment of the volume of active and passive movements. If there is a restriction in movements, describe the cause (pain, swelling, contracture, tendon rupture) and subjective sensations of the patient that arise when trying to make a movement.
Blood vessels (mandatory in comparison with the symmetrical side) is obligatory for the examination of lower limbs: a. femoralis a. poplitea, a. tibialis posterior, a. dorsalis pedis); upper limbs (a. axillaris, a. brachialis, a. ulnaris).
4. PRELIMINARY DIAGNOSIS
Based on the patient’s complaints, medical history, medical history and physical research methods (indicate examination, palpation, percussion, auscultation), a preliminary diagnosis is formulated with the leading clinical syndromes highlighted and the plan for additional examination methods defined, which lists those methods by points. laboratory and instrumental studies, which it is advisable to conduct in order to clarify this diagnosis.
5. ADDITIONAL METHODS
Some additional methods (screening) are used in the examination of all patients, regardless of the estimated diagnosis. These include general blood cell count, urine, feces, biochemical blood tests (total protein content, fractions of bilirubin, glucose, urea, coagulogram, blood group and Rh factor), chest x-ray, ECG. The choice of additional methods, those will be included in the examination plan, will depend on the estimated diagnosis. After setting out a patient examination plan in the case report, the results of laboratory and instrumental examination are presented. At the same time, the protocols of instrumental research methods (endoscopy, abdominal ultrasound, dopplerography, angiography, etc.) must be indicated with a description of changes characteristic of the disease. When using complex methods (CTI, MRI), requiring a qualified interpretation, it is enough to indicate their conclusion. Laboratory data must be provided in the SI system.
6. CLINICAL DIAGNOSIS
The diagnosis is a brief conclusion medical opinion on the origin of the disease reflecting its nosology, etiology, pathogenesis and morphofunctional manifestations, formulated in terms provided for by the adopted classifications and nomenclature of diseases. Currently, when making a clinical diagnosis, they use the "International Statistical Classification of Diseases and Health Problems" of the 10th revision (ICD-10).
6.1. Methodological foundations of the diagnosis.
By the method of construction, the following types of diagnosis: by analogy; synthetic, or complete; differential diagnosis and, as part of it, a diagnosis by exclusion; by observation; according to the therapeutic effect (diagnosis ex juvantibus); as a result of the harmful effects of drugs; during surgery. In daily clinical practice, the diagnosis is often made by analogy (direct diagnosis), by observation, by the therapeutic effect and the synthetic diagnosis.
Diagnosis by analogy - the revealed signs are compared with the symptoms of a disease known to the doctor, and with the similarity of the signs revealed in the patient, with the manifestations characteristic of a disease it is considered that the patient suffers from an identical disease.
A synthetic, or pathogenetic, diagnosis is based on the pathogenetic links of clinical manifestations and on the distinction of diseases according to their characteristic symptom complexes - syndromes. This facilitates the diagnosis of diseases and narrows the search for specific nosological forms.
After analyzing all the clinical data, the procedure for constructing a diagnosis begins, which can be divided into three stages:
a) joining of the isolated signs of the disease into syndromes for organs, systems or processes that occur in a particular organ/system. Examples: pain, dyspeptic, intoxication, icteric, syndrome of respiratory failure, etc.
b) the combination of a number of syndromes related to the defeat of one organ/system into a joint complex, pathogenetically related to each other;
c) the conversion from a group of syndromes to the concept of disease as a nosological unit.
6.2. Making a clinical diagnosis.
The diagnosis is substantiated on the basis of complaints, case history, objective examination (general and local examination, palpation, percussion, auscultation), laboratory and instrumental studies.
The clinical diagnosis should include:
a) A comprehensive diagnosis of the main disease (name of the disease; its clinical, clinical, morphological or pathogenetic form; the course; stages, phases, degree of activity; degree of functional disorders/severity);
b) The diagnosis of complications;
c) A comprehensive diagnosis of concomitant diseases.
A nosological unit is considered to be a disease characterized by typical combinations of symptoms, as well as highlighted in an independent statistical section of the ICD and having a definite etiological characteristic.
The main disease is a disease that has, at the time of assessing the patient’s condition, the most pronounced manifestations that threaten his health and/or life, and for which treatment is being carried out (i.e., determines the patient’s severity or caused hospitalization).
Complication of the main disease is a pathological process that is closely associated with the disease and significantly aggravating its course.
A concomitant disease is a nosological unit that is not associated with the main disease and its complications in pathogenesis and etiology and does not significantly affect their course.
7. TREATMENT PLAN
After making a complete clinical diagnosis, it is necessary to prescribe the appropriate treatment. This section sets out the goals, objectives, basic principles and modern methods and means of treating the disease and preventing its complications. The following treatments are available:
§ Etiological (provides for the elimination or correction of causal, provoking factors, risk factors);
§ Pathogenetic, affecting the basic mechanisms of the disease (inflammation, allergies, functional disorders, deficiency of certain factors, intoxication, etc.);
§ Symptomatic treatment aimed at stopping certain symptoms of the disease.
A treatment plan must include:
§ Life mode (strict bed, bed, ward, general). If necessary, the patient's/any part of the body forced position, the regimen must be specified (postural position, Trendelenburg, Fowler, etc.);
§ Diet (indicating the number of curative diet by Pevzner);
§ Prevention of infectious and thrombotic complications (to assess the risk factors for the development of suppurative complications, DVT and pulmonary embolism with the planned surgery and appoint appropriate measures);
§ Medications (indicating the name, concentration of the active substance, dose, route, frequency and duration of appointment); medications are given as prescriptions.
§ Surgical treatment (if necessary) with the name of the operation and the type of anesthesia and the degree of operational-anesthetic risk;
§ Physiotherapeutic treatment.
8. EPICRISE
The patient’s discharge from the hospital at the end of treatment does not always mean his complete recovery. Inpatient treatment is considered completed upon reaching a satisfactory/stable compensated condition, after which a patient is discharged either under the supervision of a polyclinic surgeon, or for outpatient treatment and rehabilitation, if necessary. In this section you must specify:
§ Complete clinical diagnosis;
§ The treatment (surgical, medication);
§ The condition dynamics and the achieved result of treatment (improvement, full recovery);
§ The course of the postoperative period, complications of the operation and the condition of the wound (if the patient was operated on);
§ Recommendations for further treatment and rehabilitation;
§ Terms of patient’s follow-up examination in outpatient management.
Suppl. 1
GLASGOW SCALE
Suppl. 2
METHODS OF ASSESSMENT OF OPERATIVE AND ANESTHESIOLOGICAL RISK