
История создания датчика движения: Первый прибор для обнаружения движения был изобретен немецким физиком Генрихом Герцем...
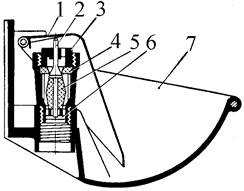
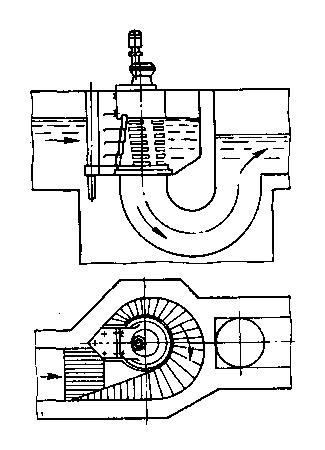
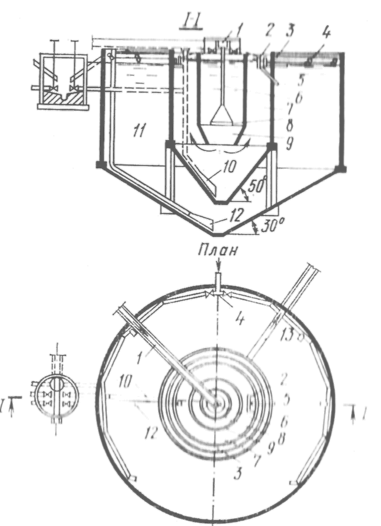
Индивидуальные и групповые автопоилки: для животных. Схемы и конструкции...
История создания датчика движения: Первый прибор для обнаружения движения был изобретен немецким физиком Генрихом Герцем...
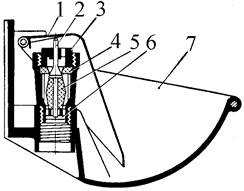
Индивидуальные и групповые автопоилки: для животных. Схемы и конструкции...
Топ:
Устройство и оснащение процедурного кабинета: Решающая роль в обеспечении правильного лечения пациентов отводится процедурной медсестре...
Установка замедленного коксования: Чем выше температура и ниже давление, тем место разрыва углеродной цепи всё больше смещается к её концу и значительно возрастает...
Характеристика АТП и сварочно-жестяницкого участка: Транспорт в настоящее время является одной из важнейших отраслей народного хозяйства...
Интересное:
Влияние предпринимательской среды на эффективное функционирование предприятия: Предпринимательская среда – это совокупность внешних и внутренних факторов, оказывающих влияние на функционирование фирмы...
Распространение рака на другие отдаленные от желудка органы: Характерных симптомов рака желудка не существует. Выраженные симптомы появляются, когда опухоль...
Отражение на счетах бухгалтерского учета процесса приобретения: Процесс заготовления представляет систему экономических событий, включающих приобретение организацией у поставщиков сырья...
Дисциплины:
|
из
5.00
|
Заказать работу |
| № | Критерии качества | Уровень достоверности доказательств | Уровень убедительности рекомендаций |
| 1. | Проведена оценка ВДП и прогнозирование «трудных дыхательных путей». Результаты оценки риска трудной масочной вентиляции, трудной установки НВУ, трудной интубации зафиксированы в истории болезни. | 3 | В-С |
| 2. | При выявлении факторов риска ТДП анестезиолог зафиксировал высокий риск ТДП в истории болезни, сформулировал основной и резервный план действий, организовал присутствие необходимых специалистов и обеспечил наличие необходимого оборудования в операционной. | 3 | В |
| 3. | Анестезиолог провел преоксигенацию 100% О2 через лицевую маску в течение не менее 3-х минут или до достижения EtO2 > 90% (при наличии мониторинга). | 3 | В |
| 4. | После безуспешных попыток интубации трахеи с помощью прямой ларингоскопии (не более 2-х попыток) анестезиолог выполнил третью попытку интубации с помощью оборудования для непрямой ларингоскопии (при наличии): видеоларингоскопов со специальными клинками с высокой кривизной для трудной интубации; оптических стилетов; гибкого интубационного эндоскопа. | 1-2 | А-В |
| 5. | После трех неудачных попыток интубации трахеи анестезиолог выполнил установку НВУ (оптимально – с дренажным каналом), обеспечил надежную защиту ВДП, эффективную вентиляцию. | 3 | В |
| 6. | В случае безуспешной интубации, безуспешной вентиляции с помощью лицевой маски и/или НВУ анестезиолог незамедлительно, не дожидаясь развития нарушений газообмена, выполнил или организовал выполнение инвазивного доступа к верхним дыхательным путям в варианте экстренной крикотиреотомии. | 3 | В |
| 7. | Перед выполнением экстубации пациента анестезиолог оценил риск развития во время анестезии нарушений проходимости ВДП и трахеи - выполнил «тест с утечкой», при наличии показаний и условий провел УЗ-исследование ВДП и трахеи, осмотр рото- и гортаноглотки (с помощью ВЛ, ФБС). | 3 | С |
Список литературы.
1. Durga P., Sahu B.P. Neurological deterioration during intubation in cervical spine disorders. Indian J Anaesth. 2014 Nov-Dec;58(6):684-92. doi: 10.4103/0019-5049.147132. PMID: 25624530; PMCID: PMC4296351.
2. Miyabe M., Dohi S., Homma E. Tracheal intubation in an infant with Treacher-Collins syndrome--pulling out the tongue by a forceps. Anesthesiology. 1985 Feb;62(2):213-4. doi: 10.1097/00000542-198502000-00037. PMID: 3970385.
3. Nargozian C. The airway in patients with craniofacial abnormalities. Paediatr Anaesth. 2004 Jan;14(1):53-9. doi: 10.1046/j.1460-9592.2003.01200.x. PMID: 14717875.
4. Buckland R.W., Pedley J. Lingual thyroid--a threat to the airway. Anaesthesia. 2000 Nov;55(11):1103-5. doi: 10.1046/j.1365-2044.2000.01610.x. PMID: 11069338.
5. Coonan T.J., Hope C.E., Howes W.J., Holness R.O., MacInnis E.L. Ankylosis of the temporo-mandibular joint after temporal craniotomy: a cause of difficult intubation. Can Anaesth Soc J. 1985 Mar;32(2):158-60. doi: 10.1007/BF03010042. PMID: 3986653.
6. Roa N.L., Moss K.S. Treacher-Collins syndrome with sleep apnea: anesthetic considerations. Anesthesiology. 1984 Jan;60(1):71-3. doi: 10.1097/00000542-198401000-00017. PMID: 6419642.
7. Greenland K.B. Airway assessment based on a three column model of direct laryngoscopy. Anaesth Intensive Care. 2010 Jan;38(1):14-9. doi: 10.1177/0310057X1003800104. PMID: 20191771.
8. Mason A.M., Rich J. Airway anatomy and assessment. In: Rich J., editor. SLAM: Street Level Airway Management. Upper Saddle River, NJ: Brady/Pearson Prentice Hall; 2007. pp. 19–36.
9. Mosier J.M., Joshi R., Hypes C., et al. The physiologically difficult airway. West J Emerg Med. 2015;16(7):1109-1117.
10. Mosier J.M.. Physiologically difficult airway in critically ill patients: winning the race between haemoglobin desaturation and tracheal intubation. Br J Anaesth. 2020;125(1):e1-e4.
11. De Jong A., Rolle A., Molinari N. et al. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: a multicenter cohort study. Crit Care Med. 2018; 46: 532-539.
12. Sakles J.C., Pacheco G.S., Kovacs G., Mosier J.M. The difficult airway refocused. Br J Anaesth. 2020 Jul;125(1):e18-e21. doi: 10.1016/j.bja.2020.04.008. Epub 2020 May 8. PMID: 32402374.
13. Kornas, Rebecca L.; Owyang, Clark G.; Sakles, John C.; Foley, Lorraine J.; Mosier, Jarrod M.; on behalf of the Society for Airway Management’s Special Projects Committee Evaluation and Management of the Physiologically Difficult Airway: Consensus Recommendations From Society for Airway Management, Anesthesia & Analgesia: February 2021 - Volume 132 - Issue 2 - p 395-405 doi: 10.1213/ANE.0000000000005233.
14. Practice Guidelines for Management of the Difficult Airway: An updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 2013; 118:251-70.
15. Cheney F.W., Posner K.L., Lee L.A., et al. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology 2006; 105:1081-1086.
16. Domino K.B., Posner K.L., Caplan R.A., Cheney F.W.: Airway injury during anesthesia: A closed claims analysis. Anesthesiology 1999; 91:1703–11.
17. Metzner J., Posner K.L., Lam M.S., Domino K.B. Closed claims’ analysis. Best Pract Res Clin Anaesthesiol 2011; 25(2):263-76.
18. Miller, C.G.: Management of the Difficult Intubation in Closed Malpractice Claims. ASA Newsletter 2000; 64(6):13-16 & 19.
19. Schroeder RA, Pollard R, Dhakal I, Cooter M, Aronson S, Grichnik K, Buhrman W, Kertai MD, Mathew JP, Stafford-Smith M: Temporal trends in difficult and failed tracheal intubation in a regional community anesthetic practice. Anesthesiology 2018; 128:502–10.
20. Joffe A.M., Aziz M.F., Posner K.L., Duggan L.V., Mincer S.L., Domino K.B. Management of Difficult Tracheal Intubation: A Closed Claims Analysis. Anesthesiology. 2019 Oct;131(4):818-829. doi: 10.1097/ALN.0000000000002815. PMID: 31584884; PMCID: PMC6779339.
21. Kheterpal S., Han R., Tremper K.K,. et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885-891.
22. Kheterpal S., Martin L., Shanks A.M., et al. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009;110:891-897.
23. Langeron O., Masso E., Huraux C., et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229-1236.
24. Samsoon G.L., Young J.R. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487-490.
25. Tachibana N., Yukitoshi N., Michiaki Y. Incidence of cannot ntubate–cannot ventilate (CICV): results of a 3-year retrospective multicenter clinical study in a network of university hospitals. J Anesth. 2015;29:326-330.
26. Martin L.D., Mhyre J.M., Shanks A.M., et al. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011;114:42-48.
27. El Ganzouri A.R., McCarthy R.J., Tuman K.J., et al. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197-1204.
28. Cook T.M., MacDougall-Davis S.R. Complications and failure of airway management. Br J Anaesth. 2012 Dec;109 Suppl 1:i68-i85.
29. Cook T.M., Woodall N., Frerk C.; Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011 May;106(5):617-31.
30. Долбнева Е.Л., Стамов В.И., Мизиков В.М., Бунятян А.А. «Трудные дыхательные пути» – частота встречаемости в РФ и пути решения». Тезисы XIV Съезда Федерации анестезиологов и реаниматологов, стр. 116-117.
31. Андреенко А.А., Братищев И.В., Долбнева Е.Л., Пиковский В.Ю., Стамов В.И.. Обеспечение проходимости верхних дыхательных путей (обзор существующей практики в РФ на 2020 год). Результаты многоцентрового исследования. Вестник интенсивной терапии им. А.И. Салтанова. 2021;1:107–115. DOI: 10.21320/1818-474X-2021-1-107-115.
32. Miller's Anesthesia, 7th Edition. By Ronald D. Miller, MD, Lars I. Eriksson, Lee A. Fleisher, MD, Jeanine P. Wiener-Kronish, MD and William L. Young, 2012. 3312 pages.
33. Алгоритмы действий при критических ситуациях в анестезиологии. Рекомендации всемирной федерации обществ анестезиологов. Под редакцией Брюса Маккормика (Bruce McCormick). Русское издание под редакцией Э.В.Недашковского. Архангельск: СГМА, – 122 с. – ISBN 978-5-85879-763-0. Главы: «План интубации трахеи», «Непредвиденно сложная интубация», «Сценарий «не могу интубировать - не могу вентилировать».
34. Анестезиология: национальное руководство/Под ред. А.А. Бунятяна, В.М. Мизикова - М.: ГЭОТАР-Медиа, 2013. - 1104 с. - (Серия "Национальные руководства"). Мизиков В.М., Долбнева Е.Л. Глава 11. Поддержание проходимости дыхательных путей и проблема «трудной интубации трахеи».
35. Буров Н.Е., Волков О.И. Тактика и техника врача-анестезиолога при трудной интубации. Клин анестезиол и реаниматол. 2004, т.1, №2, С. 68-74.
36. Буров Н.Е. Протокол обеспечения проходимости дыхательных путей. (Обзор литературы и материалов совещания главн. Анестезиологов МЗСР РФ.2005). Клин анестезиол. и реаниматол. 2005, т.2., №3, С. 2-12.
37. Молчанов И.В., Буров Н.Е., Пулина Н.Н., Черкавский О.Н. Алгоритм действия врача при трудной интубации. Клиническая практика №2, 2012: 51-57.
38. Молчанов И. В., Заболотских И. Б., Магомедов М. А.. Трудный дыхательный путь с позиции анестезиолога-реаниматолога пособие для врачей. Петрозаводск: ИнтелТек, 2006. —128 с.
39. Ellard, L., Wong, D.T. Preoperative Airway Evaluation. Curr Anesthesiol Rep 10, 19–27 (2020). https://doi.org/10.1007/s40140-020-00366-w.
40. Lundstrom L.H., Moller A.M., Rosenstock C., et al. A documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia. 2009;64:1081-1088.
41. Ferrari L.R., Bedford R.F.: General anesthesia prior to treatment of anterior mediastinal masses in pediatric cancer patients.Anesthesiology 1990; 72:991–5.
42. Zarogoulidis P., Kontakiotis T., Tsakiridis K., Karanikas M., Simoglou C., Porpodis K. Difficult airway and difficult intubation in postintubation tracheal stenosis: a case report and literature review. Ther Clin Risk Manag. 2012;8:279-86. doi: 10.2147/TCRM.S31684. Epub 2012 Jun 27. PMID: 22802693; PMCID: PMC3395408.
43. Youn A.M., Yoon S.H., Park S.Y. Failed intubation of an unanticipated postintubation tracheal stenosis: a case report. Korean J Anesthesiol. 2016 Apr;69(2):167-70. doi: 10.4097/kjae.2016.69.2.167. Epub 2016 Mar 30. PMID: 27064682; PMCID: PMC4823413.
44. Hidehiko Y., Kohno M., Nito M., Aruga N., Oiwa K., Nakagawa T., Masuda R., Iwazaki M. Postintubation tracheal stenosis 35 years after neonatal resuscitation. Int J Surg Case Rep. 2020;71:378-381. doi: 10.1016/j.ijscr.2020.02.030. Epub 2020 Feb 19. PMID: 32487473; PMCID: PMC7322740.
45. Nouraei S.A., Ma E., Patel A., Howard D.J., Sandhu G.S. Estimating the population incidence of adult post-intubation laryngotracheal stenosis. Clin Otolaryngol. 2007;32:411–412.
46. Spittle N., McCluskey A. Lesson of the week: tracheal stenosis after intubation. BMJ. 2000;321:1000–1002.
47. Gätke M.R., Wetterslev J. Danish Anaesthesia Database. Documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia 2009;64:1081-8.
48. Francon D., Bruder N. Why should we inform the patients after difficult tracheal intubation? Ann Fr Anesth Reanim 2008;27:426-30.
49. Cheney F.W., Posner K.L., Caplan R.A. Adverse respiratory events infrequently leading to malpractice suits. A closed claims analysis. Anesthesiology. 1991;75(6):932-939.
50. Peterson G.N., Domino K.B., Caplan R.A., et al. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103(1):33-39.
51. Stefan De Hert M., Sven Staender, Gerhard Fritsch, Jochen Hinkelbein, et al. Pre-operative evaluation of adults undergoing elective noncardiac surgery Updated guideline from the European Society of AnaesthesiologyEur J Anaesthesiol 2018; 35:407–465/
52. Siyam M.A., Benhamou D. Difficult endotracheal intubation in patients with sleep apnea syndrome. Anesth Analg 2002; 95:1098–1102.
53. Lundstrøm L.H., Rosenstock C.V., Wetterslev J., Nørskov A.K. The DIFFMASK score for predicting difficult facemask ventilation: a cohort study of 46,804 patients. Anaesthesia. 2019 Oct;74(10):1267-1276. doi: 10.1111/anae.14701. Epub 2019 May 20. PMID: 3110685123-24.
54. Sinha A., Jayaraman L., Punhani D. Predictors of difficult airway in the obese are closely related to safe apnea time! J Anaesthesiol Clin Pharmacol. 2020 Jan-Mar;36(1):25-30. doi: 10.4103/joacp.JOACP_164_19. Epub 2020 Feb 18. PMID: 32174653; PMCID: PMC7047673.
55. Nagappa M., Wong D.T., Cozowicz C., Ramachandran S.K., Memtsoudis S.G., Chung F. Is obstructive sleep apnea associated with difficult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PLoS One. 2018 Oct 4;13(10):e0204904. doi: 10.1371/journal.pone.0204904. PMID: 30286122; PMCID: PMC6171874.
56. Leong S.M., Tiwari A., Chung F., Wong D.T. Obstructive sleep apnea as a risk factor associated with difficult airway management - A narrative review. J Clin Anesth. 2018 Mar;45:63-68. doi: 10.1016/j.jclinane.2017.12.024. Epub 2018 Jan 4. PMID: 29291467.
57. Chung F., Yegneswaran B., Liao P., et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology.2008;108:812–821.
58. Saito T. et al. Incidence of and risk factors for difficult ventilation via a supraglottic airway device in a population of 14 480 patients from South-East Asia. Anaesthesia 2015 Jun 6; [e-pub]. (http://dx.doi.org/10.1111/anae.13153.
59. Roth D., Pace N.L., Lee A., Hovhannisyan K., Warenits A.M., Arrich J., Herkner H. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev. 2018 May 15;5:CD008874. doi: 10.1002/14651858.CD008874.pub2.
60. Khan Z.H., Mohammadi M., Rasouli M.R., et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesth Analg 2009; 109:822–824.
61. Lakhe G., Poudel H., Adhikari K.M. Assessment of Airway Parameters for Predicting Difficult Laryngoscopy and Intubation in a Tertiary Center in Western Nepal. J Nepal Health Res Counc. 2020 Jan 21;17(4):516-520. doi: 10.33314/jnhrc.v17i4.2267. PMID: 32001859.
62. Faramarzi E., Soleimanpour H., Khan Z.H., Mahmoodpoor A., Sanaie S. Upper lip bite test for prediction of difficult airway: A systematic review. Pak J Med Sci. 2018 Jul-Aug;34(4):1019-1023. doi: 10.12669/pjms.344.15364. PMID: 30190773; PMCID: PMC6115582.
63. Tremblay M.H., Williams S., Robitaille A., Drolet P. Poor visualization during direct laryngoscopy and high upper lip bite test score are predictors of difficult intubation with the GlideScope1 videolaryngoscope. Anesth Analg 2008; 106:1495–1500.
64. Roth D., Pace N.L., Lee A., Hovhannisyan K., Warenits A.M., Arrich J., Herkner H. Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia. 2019 Jul;74(7):915-928. doi: 10.1111/anae.14608. Epub 2019 Mar 6. PMID: 30843190.
65. Bhure A., Ankush A., Deshmukh P. P., Tiwari Y., Comparative study of airway assessment tests to predict difficult laryngoscopy & intubation. Indian J Clin Anaesth 2019;6(2):172-179.
66. Bansal S., Rathee S., Antil P. K., Malhotra S. K., Inderja. Assessment of difficult airway by using various bedside screening tests for endotracheal intubation. Indian J Clin Anaesth 2019;6(2):270-273.
67. Mallhi A.I., Abbas N., Naqvi S.M.N., Murtaza G., Rafique M., Alam S.S. A comparison of Mallampati classification, thyromental distance and a combination of both to predict difficult intubation. Anaesth Pain & Intensive Care 2018;22(4):468-473.
68. Wilson M.E., Spiegelhalter D., Robertson J.A., Lesser P. Predicting difficult intubation. Br J Anaesth. 1988 Aug;61(2):211-6. doi: 10.1093/bja/61.2.211. PMID: 3415893.
69. L'Hermite J., Nouvellon E., Cuvillon P., Fabbro-Peray P., Langeron O., Ripart J. The Simplified Predictive Intubation Difficulty Score: a new weighted score for difficult airway assessment. Eur J Anaesthesiol. 2009 Dec;26(12):1003-9. doi: 10.1097/EJA.0b013e32832efc71. PMID: 19593145.
70. Reed M.J., Rennie L.M., Dunn M.J., et al. Is the 'LEMON' method an easily applied emergency airway assessment tool? European Journal of Emergency Medicine: Official Journal of the European Society for Emergency Medicine. 2004 Jun;11(3):154-157. DOI: 10.1097/01.mej.0000127645.46457.b9.
71. Arne J., et al. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. Br J Anaesth, 1998. 80(2): pp. 140-6.
72. Дзядзько А. М. Повышение безопасности и эффективности анестезиологического обеспечения у больных при прогнозируемой трудной интубации трахеи: Дис.. кандидата мед. наук. Минск. 2003. 156 с.
73. Nørskov A. K., Wetterslev J., Rosenstock C. V., Afshari A., et al. Effects of using the simplified airway risk index vs usual airway assessment on unanticipated difficult tracheal intubation - a cluster randomized trial with 64,273 participants, BJA: British Journal of Anaesthesia, Volume 116, Issue 5, May 2016, Pages 680–689, https://doi.org/10.1093/bja/aew057.
74. Nørskov A.K., Rosenstock C.V., Wetterslev J., Astrup G., Afshari A., Lundstrøm L.H. Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia 2015; 70: 272–81.
75. Lim K. S., Nielsen J. R.. Objective description of mask ventilation, BJA: British Journal of Anaesthesia, Volume 117, Issue 6, December 2016, Pages 828–829, https://doi.org/10.1093/bja/aew368.
76. Nielsen J.R., Lim K.S. Increasing the Scope on Difficult Airways: What About Mask Ventilation? Anesthesia & Analgesia: September 2019 - Volume 129 - Issue 3 - p e109 doi: 10.1213/ANE.0000000000004285.
77. Bradley J.A., Urman R.D., Yao D. Challenging the Traditional Definition of a Difficult Intubation: What Is Difficult? Anesthesia and Analgesia. 2019 Mar;128 (3):584-586. DOI: 10.1213/ane.0000000000003886.
78. Baker P. Mask ventilation. F1000Res. 2018 Oct 23;7: F1000. Faculty Rev-1683. doi: 10.12688/f1000research.15742.1. PMID: 30416707; PMCID: PMC6206602.
79. Nielsen J.R., Lim K.S. Testing mask ventilation: It's capnography that counts. Acta Anaesthesiol Scand. 2020 Mar;64(3):419. doi: 10.1111/aas.13530. Epub 2019 Dec 23. PMID: 31833560.
80. Cook T.M., Nolan J.P., Verghese C., et al. Randomized crossover comparison of the proseal with the classic laryngeal mask airway in unparalysed anaesthetized patients. Br J Anaesth. 2002;88(4):527-533.
81. Cook T.M. A new practical classification of laryngeal view. Anaesthesia, 2000. 55: pp. 274-9.
82. Swann A.D., English J.D., O'Loughlin E.J. The development and preliminary evaluation of a proposed new scoring system for videolaryngoscopy. Anaesthesia and Intensive Care 2012; 40: 697–701.
83. Frederic Adnet, Stephen W. Borron, Stephane X. Racine, Jean-Luc Clemessy, Jean-Luc Fournier, Patrick Plaisance, Claude Lapandry; The Intubation Difficulty Scale (IDS): Proposal and Evaluation of a New Score Characterizing the Complexity of Endotracheal Intubation. Anesthesiology 1997; 87:1290–1297 doi: https://doi.org/10.1097/00000542-199712000-00005.
84. Mallin M., Curtis K., Dawson M., Ockerse P., Ahern M. Accuracy of ultrasound-guided marking of the cricothyroid membrane before simulated failed intubation. Am J Emerg Med 2014; 32: 61–3.
85. Ying GUO, Yufang FENG, Hui LIANG, Rubo ZHANG, Xiaolan CAI, Xinliang PAN. Role of flexible fiberoptic laryngoscopy in predicting difficult intubation. Minerva Anestesiologica 2018 March;84(3):337-45.DOI: 10.23736/S0375-9393.17.12144-9.
86. Rosenblatt W., Ianus A.I., Sukhupragarn W., Fickenscher A., Sasaki C. Preoperative endoscopic airway examination (PEAE) provides superior airway information and may reduce the use of unnecessary awake intubation. Anesth. Analg 2011;112:602-7.
87. Kanaya N., Kawana S., Watanabe H., Niiyama Y., Niiya T., Nakayama M., et al. The utility of three-dimensional computed tomography in unanticipated difficult endotracheal intubation. Anesth Analg 2000;91:752-4.
88. You-Ten, K.E., Siddiqui, N., Teoh, W.H. et al. Point-of-care ultrasound (POCUS) of the upper airway. Can J Anesth/J Can Anesth 65, 473–484 (2018). https://doi.org/10.1007/s12630-018-1064-8.
89. Kajekar P., Mendonca C., Gaur V. Role of ultrasound in airway assessment and management. Interv J Ultrasound Appl Technol Perioper Care 2010;1:97-100.
90. Zhang, Jinbin & Teoh, Wendy & Kristensen, Michael. Ultrasound in Airway Management. Current Anesthesiology Reports (2020) 10:317–326. https://doi.org/10.1007/s40140-020-00412-7.
91. Kristensen M.S. Ultrasonography in the management of the airway. Acta Anaesthesiol Scand 2011;55:1155-73.
92. Prasad A., Yu E., Wong D.T., Karkhanis R., Gullane P., Chan V.W. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J Ultrasound Med 2011;30:965-72.
93. Sustic A., Miletic D., Protic A., Ivancic A., Cicvaric T. Can ultrasound be useful for predicting the size of a left double-lumen bronchial tube? Tracheal width as measured by ultrasonography versus computed tomography. J Clin Anesth 2008;20:247-52.
94. Lakhal K., Delplace X., Cottier J.P., Tranquart F., Sauvagnac X., Mercier C., et al. The feasibility of ultrasound to assess subglottic diameter. Anesth Analg 2007;104:611-4.
95. Ezri T., Gewürtz G., Sessler D.I., Medalion B., Szmuk P., Hagberg C., et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia 2003;58:1111-4.
96. Kundra P., Mishra S.K., Ramesh A. Ultrasound of the airway. Indian J Anaesth 2011;55:456-62.
97. Ni, H., Guan, C., He, G. et al. Ultrasound measurement of laryngeal structures in the parasagittal plane for the prediction of difficult laryngoscopies in Chinese adults. BMC Anesthesiol 20, 134 (2020). https://doi.org/10.1186/s12871-020-01053-3.
98. Gupta M., Sharma S., Katoch S. An observational study to evaluate the role of ultrasound in the prediction of difficult laryngoscopy. Bali J Anaesthesiol 2020;4:172-7.
99. Yadav U., Singh R.B., Chaudhari S., Srivastava S. Comparative study of preoperative airway assessment by conventional clinical predictors and ultrasound-assisted predictors. Anesth Essays Res 2020;14:213-8.
100. Parameswari A., Govind M., Vakamudi M. Correlation between preoperative ultrasonographic airway assessment and laryngoscopic view in adult patients: A prospective study. J Anaesthesiol Clin Pharmacol 2017;33:353-8.
101. Alessandri F., Antenucci G., Piervincenzi E., Buonopane C., Bellucci R, Andreoli C., et al. Ultrasound as a new tool in the assessment of airway difficulties: an observational study. Eur J Anaesthesiol.2019;36(7):509–15.
102. Abdelhady, Baher & Elrabiey, M. & Elrahman, A. & Mohamed, E.. (2020). Ultrasonography versus conventional methods (Mallampati score and thyromental distance) for prediction of difficult airway in adult patients. Egyptian Journal of Anaesthesia. 36. 83-89. 10.1080/11101849.2020.1768631.
103. Wojtczak J.A. Submandibular sonography: Assessment of hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable sonography. J Ultrasound Med 2012;31:523-8.
104. Gupta S., Rajesh K.R., Jain D. Airway assessment: Predictors of difficult airway. Indian J Anesth 2005;49:257-62.
105. Jain K., Yadav M., Gupta N., Thulkar S., Bhatnagar S. Ultrasonographic assessment of airway. J Anaesthesiol Clin Pharmacol. 2020 Jan-Mar;36(1):5-12. doi: 10.4103/joacp.JOACP_319_18. Epub 2020 Feb 18. PMID: 32174650; PMCID: PMC7047677.
106. Petrisor C., Dîrzu D., Trancă S., Hagău N., Bodolea C. Preoperative difficult airway prediction using suprahyoid and infrahyoid ultrasonography derived measurements in anesthesiology. Med Ultrason. 2019 Feb 17;21(1):83-88. doi: 10.11152/mu-1764. PMID: 30779836.
107. Imran Nazir."A Comparative Correlation Of Pre-Anaesthetic Airway Assessment Using Ultrasound With Cormack Lehane Classification Of Direct Laryngoscopy". IOSR Journal of Dental and Medical Sciences (IOSR-JDMS), vol. 17, no. 4 2018, pp 43-51.
108. Koundal V., Rana S., Thakur R., Chauhan V., Ekke S., Kumar M. The usefulness of point of care ultrasound (POCUS) in preanaesthetic airway assessment. Indian J Anaesth. 2019 Dec; 63(12):1022-1028. doi: 10.4103/ija.IJA_492_19. Epub 2019 Dec 11. PMID: 31879427; PMCID: PMC6921326.
109. Bianchini A., Nardozi L., Nardi E., Scuppa M.F. Airways ultrasound in predicting difficult face mask ventilation. Minerva Anestesiol 2021;87:26-34. DOI: 10.23736/S0375-9393.20.14455-9.
110. Rana S., Verma V., Bhandari S., Sharma S., Koundal V., Chaudhary S.K. Point-of-care ultrasound in the airway assessment: A correlation of ultrasonography-guided parameters to the Cormack-Lehane Classification. Saudi J Anaesth. 2018 Apr-Jun;12(2):292-296. doi: 10.4103/sja.SJA_540_17. PMID: 29628843; PMCID: PMC5875221.
111. Bektas F., Soyuncu S., Yigit O., Turhan M. Sonographic diagnosis of epiglottal enlargement. Emerg Med J 2010;27:224-5.
112. Werner S.L., Jones R.A., Emerman C.L. Sonographic assessment of the epiglottis. Acad Emerg Med 2004;11:1358-60.
113. Kristensen M.S., Teoh W.H., Graumann O., Laursen C.B. Ultrasonography for clinical decision-making and intervention in airway management: From the mouth to the lungs and pleurae. Insights Imaging 2014;5:253-79.
114. Halder, Bivash & N, Anil & Rajaram, Narayanan & Rajkumar, V & Krishna, Harini. (2020). Ultrasound guided airway assessment- an observational study to correlate airway parameter to cormack-lehane grading of laryngoscopy. Indian Journal of Clinical Anaesthesia. 7. 657-661.
115. Turkay Aydogmus M., Erkalp K., Nadir Sinikoglu S., Usta T.A., O Ulger G., Alagol A. Is ultrasonic investigation of transverse tracheal air shadow diameter reasonable for evaluation of difficult airway in pregnant women: A prospective comparative study. Pak J Med Sci 2014;30:91-5.
116. Gupta K., Gupta P.K., Rastogi B., Krishan A., Jain M., Garg G. Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res 2012;6:157-60.
117. Shibasaki M., Nakajima Y., Ishii S., Shimizu F., Shime N., Sessler D.I. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology 2010;113:819-24.
118. Kristensen M.S. Ultrasonography in airway management. In: Hagberg C, editor. Benumof and Hagberg’s Airway Management. 3rd ed. Philadelphia: Elsevier Saunders; 2012. p. 76-91.
119. Kristensen M.S., Teoh W.H., Rudolph S.S. Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact. Br J Anaesth 2016; 117(Suppl 1): i39-48.
120. Siddiqui N., Arzola C., Friedman Z., Guerina L., You-Ten K.E. Ultrasound improves cricothyrotomy success in cadavers with poorly defined neck anatomy: a randomized control trial. Anesthesiology 2015; 123: 1033-41.
121. Even-Tov E., Koifman I., Rozentsvaig V., Livshits L., Gilbey P. Pre-procedural ultrasonography for tracheostomy in critically ill patients: a prospective study. Isr Med Assoc J 2017; 19: 337-40.
122. Kristensen M.S., Teoh W.H., Rudolph S.S., et al. Structured approach to ultrasound-guided identification of the cricothyroid membrane: a randomized comparison with the palpation method in the morbidly obese. Br J Anaesth 2015; 114: 1003-4.
123. Shime N., Ono A., Chihara E., Tanaka Y. Current status of pulmonary aspiration associated with general anesthesia: a nationwide survey in Japan. Masui. 2005 Oct; 54(10):1177-85.
124. Engelhardt T., Webster N.R. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999;83:453–460.
125. Cook T.M. Strategies for the prevention of airway complications – a narrative review. Anaesthesia 2018; 73: 93–111.
126. Sakai T., Planinsic R.M., Quinlan J.J., Handley L.J., Kim T.Y., Hilmi I.A. The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis. Anesth Analg 2006; 103: 941 –7.
127. Sharma G., Jacob R., Mahankali S., Ravindra M.N. Preoperative assessment of gastric contents and volume using bedside ultrasound in adult patients: A prospective, observational, correlation study. Indian J Anaesth. 2018 Oct;62(10):753-758. doi: 10.4103/ija.IJA_147_18. PMID: 30443057; PMCID: PMC6190418.
128. Garg H., Podder S., Bala I., Gulati A.. Comparison of fasting gastric volume using ultrasound in diabetic and non-diabetic patients in elective surgery: An observational study. Indian J Anaesth. 2020 May;64(5):391-396. doi: 10.4103/ija.IJA_796_19. Epub 2020 May 1. PMID: 32724247; PMCID: PMC7286410.
129. Perlas A., Davis L., Khan M., Mitsakakis N., Chan V.W.S. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg.2011;113(1):93e97.
130. Perlas A., Mitsakakis N., Liu L., Cino M., Haldipur N., Davis L., Cubillos J., Chan V. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination.Anesth Analg. 2013 Feb; 116(2):357-63.
131. Bouvet L., Mazoit JX, Chassard D, Allaouchiche B, Boselli E, Benhamou D. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume. Anesthesiology. 2011; 114: 1086-1092.
132. Perlas A. Diagnostic Accuracy of Point-of-Care Gastric Ultrasound. Anesth Analg. 2019 Jan;128(1):89-95. doi: 10.1213/ANE.0000000000003372. PMID: 29624530.
133. Alakkad H., Kruisselbrink R., Chin K.J. et al. Point-of-care ultrasound defines gastric content and changes the anesthetic management of elective surgical patients who have not followed fasting instructions: a prospective case series. Can J Anesth 2015; 62: 1188e95.
134. Gagey A..C, de Queiroz Siqueira M., Monard C., Combet S., et al. The effect of pre-operative gastric ultrasound examination on the choice of general anaesthetic induction technique for non-elective paediatric surgery. A prospective cohort study. Anaesthesia. 2018 Mar;73(3):304-312. doi: 10.1111/anae.14179. Epub 2017 Dec 19. PMID: 29265174.
135. Zhang G., Huang X., Shui Y., Luo C., Zhang L. Ultrasound to guide the individual medical decision by evaluating the gastric contents and risk of aspiration: A literature review. Asian J Surg. 2020 Dec;43(12):1142-1148. doi: 10.1016/j.asjsur.2020.02.008. Epub 2020 Mar 11. PMID: 32171605.
136. Van de Putte P., Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014 Jul;113(1):12-22. doi: 10.1093/bja/aeu151. Epub 2014 Jun 3. PMID: 24893784.
137. El-Boghdadly K., Wojcikiewicz T., Perlas A. Perioperative point-of-care gastric ultrasound. BJA Educ. 2019 Jul;19(7):219-226. doi: 10.1016/j.bjae.2019.03.003. Epub 2019 Apr 24. PMID: 33456894; PMCID: PMC7808010.
138. Benhamou D. Ultrasound assessment of gastric contents in the perioperative period: Why is this not part of our daily practice? Br J Anaesth. 2015;114:545–8
139. Van de Putte P., Vernieuwe L., Bouvet L. Gastric ultrasound as an aspiration risk assessment tool. Indian J Anaesth. 2019 Feb;63(2):160-161. doi: 10.4103/ija.IJA_756_18. PMID: 30814762; PMCID: PMC6383467.
140. Jain K, Gupta N., Yadav M., Thulkar S., Bhatnagar S. Radiological evaluation of airway – What an anaesthesiologist needs to know!. Indian J Anaesth 2019;63:257-64.
141. Bellhouse C.P., Doré C. Criteria for estimating likelihood of difficulty of endotracheal intubation with the Macintosh laryngoscope. Anaesth Intensive Care 1988;16:329-37.
142. Han Y.Z., Tian Y., Zhang H., Zhao Y.Q., Xu M., Guo X.Y. Radiologic indicators for prediction of difficult laryngoscopy in patients with cervical spondylosis. Acta Anaesthesiol Scand 2018;62:474-82.
143. Gupta K., Gupta P.K. Assessment of difficult laryngoscopy by electronically measured maxillo-pharyngeal angle on lateral cervical radiograph: A prospective study. Saudi J Anaesth 2010;4:158-62.
144. Becker M., Burkhardt K., Dulguerov P., Allal A. Imaging of the larynx and hypopharynx. Eur J Radiol 2008;66:460–479.
145. Taha M.S., Mostafa B.E., Fahmy M., Ghaffar M.K., Ghany E.A. Spiral CT virtual bronchoscopy with multiplanar reformatting in the evaluation of post-intubation tracheal stenosis: comparison between endoscopic, radiological and surgical findings. Eur Arch Otorhinolaryngol 2009;266:863–866.
146. Hoppe H., Walder B., Sonnenschein M., Vock P., Dinkel H.P. Multidetector CT virtual bronchoscopy to grade tracheobronchial stenosis. AJR Am J Roentgenol 2002;178:1195–1200.
147. Koren A., Groselj L.D., Fajdiga I. CT comparison of primary snoring and obstructive sleep apnea syndrome: role of pharyngeal narrowing ratio and soft palate-tongue contact in awake patient. Eur Arch Otorhinolaryngol 2009;266:727–734.
148. Kuo G.P., Torok C.M, Aygun N, Zinreich SJ. Diagnostic imaging of the upper airway. Proc Am Thorac Soc. 2011 Mar;8(1):40-5. doi: 10.1513/pats.201004-032RN. PMID: 21364220.
149. El-Naga H.A.A, El-Rasheedy A.I., Abdelaziz M., Shawky M. (2016) The Role of Multidetector CT Virtual Bronchoscopy in Assessment of Patients with Laryngotracheal Stenosis. J Otolaryngol ENT Res 5(2): 00135. DOI: 10.15406/joentr.2016.05.00135.
150. Naguib M., Malabarey T., AlSatli R.A., Al Damegh S., Samarkandi A.H. Predictive models for difficult laryngoscopy and intubation. A clinical, radiologic and three-dimensional computer imaging study. Can J Anaesth 1999;46:748-59.
151. Saito K., Sunouchi A., Toyama H., Yamauchi M. Preoperative Assessment of Airway Patency During General Anesthesia in a Patient With Severe Tracheal Stenosis: Effectiveness of Noninvasive Positive Pressure Ventilation. J Cardiothorac Vasc Anesth. 2020 Feb;34(2):566-567. doi: 10.1053/j.jvca.2019.06.034. Epub 2019 Jun 28. PMID: 31345712.
152. Gutiérrez J.C., Merino S., De la Calle P., Perrino C., Represa M., Moral P. Correlation of Preoperative Findings in the Computerized Axial Tomography with the Presence of Via Difficult Airway in Patients Operated Through Otorhinolaryngological Surgery of the Head and Neck. Rev Esp Anestesiol Reanim. 2018 May;65(5):252-257. DOI: 10.1016/j.redar.2018.01.013.
153. Verma, Sunil & Smith, Marshall & Dailey, Seth. (2012). Transnasal tracheoscopy. The Laryngoscope. 122. 1326-30. 10.1002/lary.23221.
154. Gemma M., Buratti L., Di Santo D., Calvi M.R., Ravizza A., Bondi S., Bussi M., Beretta L. Pre-operative transnasal endoscopy as a predictor of difficult airway: A prospective cohort study. Eur J Anaesthesiol. 2020 Feb;37(2):98-104. doi: 10.1097/EJA.0000000000001127. PMID: 31789897.
155. Gaszynski T. A comparison of pre-operative transnasal flexible endoscopic laryngoscopy and actual laryngeal view obtained with videolaryngoscopy in predicted difficult intubations. Eur J Anaesthesiol. 2021 Feb 1;38(2):201-202. doi: 10.1097/EJA.0000000000001255. PMID: 33394801.
156. Rochlin D. H., S. Moshrefi, C. Sheckter, Y. L. Karanas. Preventing Unnecessary Intubations: Use of Flexible Fiberoptic Laryngoscopy for Airway Evaluation in Patients with Suspected Airway or Inhalation Injury, Journal of Burn Care & Research, Volume 39, Issue suppl_1, April 2018, Page S7, https://doi.org/10.1093/jbcr/iry006.010.
157. Rosenblatt W., Ianus A., Sukhupragarn W., Fickenscher A., Sasaki C. Preoperative Endoscopic Airway Examination (PEAE) provides superior airway information and reduces the use of unnecessary awake intubation. Anesth Analg 2011;112:602–7.
158. Akça, Ozan; Lenhardt, Rainer; Heine, Michael F. Can Transnasal Flexible Fiberoptic Laryngoscopy Contribute to Airway Management Decisions?, Anesthesia & Analgesia: March 2011 - Volume 112 - Issue 3 - p 519-520 doi: 10.1213/ANE.0b013e31820a146d.
159. Tasli H., Karakoc O., Birkent H. A Grading System for Transnasal Flexible Laryngoscopy. J Voice. 2019 Sep;33(5):712-715. doi: 10.1016/j.jvoice.2018.02.019. Epub 2018 May 2. PMID: 29730193.
160. Weingart S.D., Levitan R.M. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med.2012; 59: 165–75.
161. Tanoubi I., Drolet P., Donati F. Optimizing preoxygenation in adults. Can J Anaesth 2009; 56: 449–66.
162. Nimmagadda, Usharani MD*†; Salem, M. Ramez MD*†; Crystal, George J. PhD† Preoxygenation: Physiologic Basis, Benefits, and Potential Risks, Anesthesia & Analgesia: February 2017 - Volume 124 - Issue 2 - p 507-517 doi: 10.1213/ANE.0000000000001589.
163. Pandey M., Ursekar R., Aphale S. Three minute tidal breathing – a gold standard techniques for pre-oxygenation for elective surgeries. Innov J Med Health Sci. 2014; 4: 194–7.
164. Gambee A.M., Hertzka R.E., Fisher D.M.: Preoxygenation techniques: Comparison of three minutes and four breaths. Anesth Analg 1987; 66:468–70.
165. Choinière A., Girard F., Boudreault D., Ruel M., Girard D.C.: Voluntary hyperventilation before a rapid-sequence induction of anesthesia does not decrease postintubation PaCO2. Anesth Analg. 2001, 93:1277-1280. 10.1097/00000539-200111000-00050.
166. Baraka A.S., Taha S.K., Aouad M.T., El-Khatib M.F., Kawkabani N.I. Preoxygenation: comparison of maximal breathing and tidal volume breathing techniques. Anesthesiology 1999;91:612-6.
167. McCrory J.W., Matthews J.N.: Comparison of four methods of preoxygenation. Br J Anaesth. 1990, 64:571-576. 10.1093/bja/64.5.571.
168. Tanoubi I., Drolet P., Donati F. Optimizing preoxygenation in adults. Can J Anaesth 2009; 56: 449–66.
169. Scheeren T.W.L., Belda F.J., Perel A. The oxygen reserve index (ORI): a new tool to monitor oxygen therapy. J Clin Monit Comput. 2018 Jun;32(3):379-389. doi: 10.1007/s10877-017-0049-4. Epub 2017 Aug 8. Erratum in: J Clin Monit Comput. 2018 Feb 14: PMID: 28791567; PMCID: PMC5943373.
170. Chen S.T., Min S. Oxygen reserve index, a new method of monitoring oxygenation status: what do we need to know? Chin Med J (Engl). 2020 Jan 20;133(2):229-234. doi: 10.1097/CM9.0000000000000625. PMID: 31904726; PMCID: PMC7028177.
171. Bell M.D.D. Routine pre-oxygenation – a new ‘minimum standard’ of care? Anaesthesia 2004; 59: 943–5.
172. McGowan P., Skinner A. Preoxygenation—the importance of a good face mask seal. Br J Anaesth1995; 75: 777–8.
173. Benumof JL. Preoxygenation: best method for both efficacy and efficiency. Anesthesiology. 1999;91:603605.
174. Goldberg M.E., Norris M.C., Larijani G.E., Marr A.T., Seltzer J.L.: Preoxygenation in the morbidly obese: A comparison of two techniques. Anesth Analg 1989; 68:520–2.
175. Dixon B.J., Dixon J.B., Carden J.R., et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology 2005; 102: 1110-5.89.
176. Altermatt F.R., Munoz H.R., Delfino A.E., Cortinez L.I. Preoxygenation in the obese patient: effects of position on tolerance to apnoea. Br J Anaesth 2005; 95: 706-9.
177. Shah U., Wong J., Wong D.T., Chung F. Preoxygenation and intraoperative ventilation strategies in obese patients: a comprehensive review. Curr Opin Anaesthesiol 2016; 29:109–118. doi: 10.1097/ACO.0000000000000267.
178. Harbut P., Gozdzik W., Stjernfält E., Marsk R., Hesselvik J.F. Continuous positive airway pressure/pressure support pre-oxygenation of morbidly obese patients. Acta Anaesthesiol Scand. 2014 Jul;58 (6):675-80. doi: 10.1111/aas.12317. Epub 2014 Apr 16.
179. Sreejit M.S., Ramkumar V. Effect of positive airway pressure during pre-oxygenation and induction of anaesthesia upon safe duration of apnoea. Indian J Anaesth 2015;59:216-21.
180. Gander S., Frascarolo P., Suter M., Spahn D.R. Magnusson, Lennart. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 2005; 100: 580–4.
181. Тanoubi I., Drolet P., Fortier L.P., Donati F. Inspiratory support versus spontaneous breathing during preoxygenation in healthy subjects. A randomized, double blind, cross-over trial]. Ann Fr Anesth Reanim 2010;29:198-203.
182. Pillai A., Daga V., Lewis et al. High –flow humidified nasal oxygenation vs standard oxygenation. Anaesthesia 2016; 71:1280-128332.
183. Elena Bignami, Francesco Saglietti, Alessandro Girombelli, Andrea Briolini, Tiziana Bove, Luigi Vetrugno, Preoxygenation during induction of anesthesia in non-critically ill patients: A systematic review, Journal of Clinical Anesthesia,Volume 52,2019,Pages 85-90,ISSN 0952-8180,https://doi.org/10.1016/j.jclinane.2018.09.008.
184. Coussa M., Proietti S., Schnyder P., et al. Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg. 2004;98(5):1491-1495.
185. El-Khatib M.F., Kanazi G., Baraka A.S. Noninvasive bilevel positive airway pressure for preoxygenation of the critically ill morbidly obese patient. Can J Anaesth. 2007;54:744–747.
186. Delay J.M., Sebbane M., Jung B., et al. The effectiveness of noninvasive positive pressure ventilation to enhance preoxygenation in morbidly obese patients: a randomized controlled study. Anesth Analg. 2008;107 (5):1707-1713.
187. Heinrich S., Horbach T., Stubner B., Prottengeier J., Irouschek A., et al. Benefits of Heated and Humidified High Flow Nasal Oxygen for Preoxygenation in Morbidly Obese Patients Undergoing Bariatric Surgery: A Randomized Controlled Study. J Obes Bariatrics. 2014;1(1): 7.
188. Patel A., Nouraei S.A.R. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015;70:323-9.
189. Badiger S., John M., Fearnley R.A., Ahmad I. Optimizing oxygenation and intubation conditions during awake fibre-optic intubation using a high-flow nasal oxygen-delivery system. Br J Anaesth 2015;115:629-32.
190. Ritchie J.E., Williams A.B., Gerard C., Hockey H. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011;39:1103–1110.
191. Mosier J.M., Hypes C.D., Sakles J.C. Understanding preoxygenation and apneic oxygenation during intubation in the critically ill. Intensive Care Med 2017; 43:226–228. doi: 10.1007/s00134-016-4426-0.
192. McNarry A.F., Patel A. The evolution of airway management - new concepts and conflicts with traditional practice. Br J Anaesth 2017; 119:i154–i166. doi: 10.1093/bja/aex385.
193. White L.D., Melhuish T.M., White L.K., Wallace L.A. Apnoeic oxygenation during intubation: a systematic review and meta-analysis. Anaesthesia and intensive care. 2017; 45(1):21-27.
194. Doyle A.J., et al. Preoxygenation and apneic oxygenation using transnasal humidified rapid-insufflation ventilatory exchange for emergency intubation. J Crit Care 2016; 36: 8–12.
195. Weingart S.D. Levitan R.M. Preoxygenation and prevention of desaturation during emergency airway management.. Ann Emerg Med. 2012; 59: 165-175.
196. Gleason J.M.., Christian B.R., Barton E.D. Nasal Cannula Apneic Oxygenation Prevents Desaturation During Endotracheal Intubation: An Integrative Literature Review. West J Emerg Med. 2018 Mar;19(2):403-411. doi: 10.5811/westjem.2017.12.34699. Epub 2018 Feb 22. PMID: 29560073; PMCID: PMC5851518.
197. Wimalasena Y., Burns B., Reid C., Ware S., Habig K. Apneic oxygenation was associated with decreased desaturation rates during rapid sequence intubation by an Australian helicopter emergency medicine service. Ann Emerg Med. 2015 Apr;65(4):371-6. doi: 10.1016/j.annemergmed.2014.11.014. Epub 2014 Dec 20. PMID: 25536868.
198. Ramachandran S.K, Cosnowski A., Shanks A., Turner C.R. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J. Clin. Anesth. 2010; 22: 164–8. 36.
199. Levitan R.M. NO DESAT! Nasal oxygen during efforts securing a tube. Emergency Physicians Monthly. 2010. [Updated 9 Dec 2010; cited 28 Mar 2015.] Available from URL: http://www.epmonthly.com/archives/ features/no-desat-/.
200. Heard A., Toner A.J., Evans J.R., Palacios A.M., Lauer S. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of Buccal RAE tube oxygen administration. Anesth Analg 2017; 124: 1162–7.
201. Oliveira J E Silva L., Cabrera D., Barrionuevo P. Effectiveness of Apneic Oxygenation During Intubation: A Systematic Review and Meta-Analysis. Annals of emergency medicine. 2017; 70(4):483-494.e11.
202. Flin, R. Human factors in the development of complications of airway management: preliminary evaluation of an interview tool / R. Flin, [et al.] // Anaesthesia. - 2013. - Vol. 68. - P. 817-825.
203. Cook T.M., Woodall N., Frerk C. Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011 May;106(5):617-31. doi: 10.1093/bja/aer058. Epub 2011 Mar 29. PMID: 21447488.
204. Greenland K.B., Acott C., Segal R., Goulding G., Riley R.H., Merry A.F. Emergency surgical airway in life-threatening acute airway emergencies--why are we so reluctant to do it? Anaesth Intensive Care. 2011 Jul;39(4):578-84. doi: 10.1177/0310057X1103900407. PMID: 21823373.
205. Fletcher G., McGeorge P., Flin R., Glavin R., Maran N. The role of nontechnical skills in anaesthesia: A review of current literature. Br J Anaesth. 2002; 88 3: 418– 29.
206. Coyle M., Martin D., McCutcheon K. Interprofessional simulation training in difficult airway management: a narrative review. Br J Nurs. 2020 Jan 9;29(1):36-43. doi: 10.12968/bjon.2020.29.1.36. PMID: 31917949.
207. Grande B., Kolbe M., Biro P. Difficult airway management and training: simulation, communication, and feedback. Curr Opin Anaesthesiol. 2017 Dec;30(6):743-747. doi: 10.1097/ACO.0000000000000523. PMID: 28957878.
208. Stringer K.R., Bajenov S., Yentis S.M.: Training in airway management. Anaesthesia 2002; 57:967–83 62.
209. Klock A.P.: Airway simulators and mannequins: A case of high infidelity? Anesthesiology 2012; 116: 1179–80.
210. Kennedy C.C., Cannon E.K., Warner D.O., Cook D.A.: Advanced airway management simulation training in medical education: A systematic review and meta-analysis. Crit Care Med 2014; 42:169–78.
211. Yang D., Wei Y.K., Xue F.S, Deng X.M., Zhi J. Simulation-based airway management training: application and looking forward Simulation-based airway management training: application and looking forward. J Anesth. 2016 Apr; 30(2):284-9.
212. Myatra S.N., Kalkundre R.S., Divatia J.V. Optimizing education in difficult airway management: meeting the challenge. Curr Opin Anaesthesiol. 2017 Dec;30(6):748-754. doi: 10.1097/ACO.0000000000000515. PMID: 28938303.
213. Lilot M., Evain J.N., Vincent A., Gaillard G., Chassard D. et. al. Simulação de manejo de via aérea difícil para residentes: estudo comparativo prospectivo [Simulation of difficult airway management for residents: prospective comparative study]. Rev Bras Anestesiol. 2019 Jul-Aug;69(4):358-368. Portuguese. doi: 10.1016/j.bjan.2019.02.002. Epub 2019 Jul 29. PMID: 31371173.
214. Bittner E.A., Schmidt U. Examining the Learning Practice of Emergency Airway Management Within an Academic Medical Center: Implications for Training and Improving Outcomes. J Med Educ Curric Dev. 2020 Oct 14;7:2382120520965257. doi: 10.1177/2382120520965257. PMID: 33134549; PMCID: PMC7576904.
215. Boet S., Bould M.D., Schaeffer R. et al. Learning fiberoptic intubation with a virtual computer program transfers to “hands on” improvement. Eur J Anaesthesiol. 2010; 27 1: 31– 5.
216. Marsland C., Larsen P., Segal R. et al. Proficient manipulation of fibreoptic bronchoscope to carina by novices on first clinical attempt after specialized bench practice. Br J Anaesth. 2010; 104 3: 375– 81.
217. Goldmann K., Steinfeldt T. Acquisition of basic fiberoptic intubation skills with a virtual reality airway simulator. J Clin Anesth. 2006; 18 2: 173– 8.
218. Davoudi M., Colt H.G. Bronchoscopy simulation: A brief review. Adv Health Sci Educ Theory Pract. 2009; 14 2: 287– 96.
219. Greif R., Egger L., Basciani R.M., Lockey A., Vogt A. Emergency skill training – A randomized controlled study on the effectiveness of the 4-stage approach compared to traditional clinical teaching. Resuscitation. 2010; 81 12: 1692– 7.
220. You-Ten K.E., Bould M.D., Friedman Z., Riem N., Sydor D., Boet S.: Cricothyrotomy training increases adherence to the ASA difficult airway algorithm in a simulated crisis: A randomized controlled trial. Can J Anaesth 2015; 62:485–94.
221. Vincent Hubert, Antoine Duwat, Romain Deransy, Yazine Mahjoub, Hervé Dupont; Effect of Simulation Training on Compliance with Difficult Airway Management Algorithms, Technical Ability, and Skills Retention for Emergency Cricothyrotomy. Anesthesiology 2014; 120:999–1008 doi: https://doi.org/10.1097/ALN.0000000000000138.
222. Naik V.N., Brien S.E. Review article: simulation: a means to address and improve patient safety Can J Anaesth. 2013 Feb; 60(2):192-200.
223. Boet S., Borges B.C., Naik V.N., Siu L.W., Riem N., Chandra D., Bould M.D., Joo H.S. Complex procedural skills are retained for a minimum of 1 yr after a single high-fidelity simulation training session. Br J Anaesth. 2011 Oct; 107(4):533-9.
224. Kuduvalli P.M., Jervis A., Tighe S.Q., Robin N.M. Unanticipated difficult airway management in anaesthetized patients: a prospective study of the effect of mannequin training on management strategies and skill retention. Anaesthesia. 2008;63:364–9.
225. Chopra, V. Does training on an anaesthesia simulator lead to improvement in performance? / V. Chopra [et al.] // Br. J. Anaesth. - 1994. - № 73 (3). - Р. 293-297.
226. Yee, B. Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education / B. Yee, [et al.] // Anesthesiology. - 2005. - Vol. 103 (2). - P. 241-248.
227. Leeper W.R., Haut E.R., Pandian V., Nakka S., Dodd-O. J, et al. Multidisciplinary Difficult Airway Course: An Essential Educational Component of a Hospital-Wide Difficult Airway Response Program. J Surg Educ. 2018 Sep-Oct;75(5):1264-1275. doi: 10.1016/j.jsurg.2018.03.001. Epub 2018 Apr 5. PMID: 29628333.
228. Sun, Y., Pan, C., Li, T. et al. Airway management education: simulation based training versus non-simulation based training-A systematic review and meta-analyses. BMC Anesthesiol 17, 17 (2017). https://doi.org/10.1186/s12871-017-0313-7.
229. Андреенко А.А., Арсентьев Л.В., Цыганков К.А., Щеголев А.В. Эффективность высокореалистичной симуляции при обучении клинических ординаторов современным алгоритмам решения проблемы «трудных дыхательных путей» // Вестник Российской Военно-медицинской академии. - 2019. - Т. 66. - №2. - C. 228-232. doi: 10.17816/brmma25950.
230. Kristensen M.S., Teoh W.H., Baker P.A. Percutaneous emergency airway access; prevention, preparation, technique and training. Br J Anaesth. 2015 Mar;114(3):357-61. doi: 10.1093/bja/aev029. PMID: 25694555.
231. Adhikari S., Situ-LaCasse E., Acuña J., Irving S., Weaver C., Samsel K., Biffar D.E., Motlagh M., Sakles J. Integration of Pre-intubation Ultrasound into Airway Management Course: A Novel Training Program. Indian J Crit Care Med. 2020 Mar;24(3):179-183. doi: 10.5005/jp-journals-10071-23370. PMID: 32435096; PMCID: PMC7225761.
232. https://www.esaic.org/patient-safety/anaesthetic-crisis-manual/.
233. Cirimele J., Cirimele J., Wu L., Chu L., Harrison K., Card S., Klemmer S. Interactive Cognitive Aids for Critical Events in Anesthesia. Lippincott, Williams and Wilkins. 2013: 13–14.
234. David L. Hepner, Alexander F. Arriaga, Jeffrey B. Cooper, Sara N. Goldhaber-Fiebert, David M. Gaba, William R. Berry, Daniel J. Boorman, Angela M. Bader; Operating Room Crisis Checklists and Emergency Manuals. Anesthesiology 2017; 127:384–392 doi: https://doi.org/10.1097/ALN.0000000000001731.
235. Forristal C., Hayman K., Smith N., Mal S., Columbus M., Farooki N., Van Aarsen K., McLeod S., Ouellette D. Does utilization of an intubation safety checklist reduce omissions during simulated resuscitation scenarios: a multi-center randomized controlled trial. CJEM. 2021 Jan;23(1):45-53. doi: 10.1007/s43678-020-00010-w. Epub 2020 Dec 18. PMID: 33683616; PMCID: PMC7747776.
236. Smith K.A., High K., Collins S.P., Self W.H. A preprocedural checklist improves the safety of emergency department intubation of trauma patients. Acad Emerg Med. 2015 Aug; 22(8):989-92.
237. Thomassen Ø., Brattebø G., Søfteland E., Lossius H.M., Heltne J.K. The effect of a simple checklist on frequent pre-induction deficiencies. Acta Anaesthesiol Scand. 2010 Nov; 54(10):1179-84.
238. Long E., Fitzpatrick P., Cincotta D.R., Grindlay J., Barrett M.J. A randomised controlled trial of cognitive aids for emergency airway equipment preparation in a Paediatric Emergency Department. Scand J Trauma Resusc Emerg Med. 2016 Jan 27;24:8. doi: 10.1186/s13049-016-0201-z. PMID: 26817789; PMCID: PMC4730650.
239. Ballow S.L., Kaups K.L., Anderson S., Chang M. A standardized rapid sequence intubation protocol facilitates airway management in critically injured patients. J Trauma Acute Care Surg. 2012 Dec; 73(6):1401-5.
240. Turner J.S., Bucca A.W., Propst S.L., Ellender T.J., Sarmiento E.J., Menard L.M., Hunter B.R. Association of Checklist Use in Endotracheal Intubation With Clinically Important Outcomes: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020 Jul 1;3(7):e209278. doi: 10.1001/jamanetworkopen.2020.9278. Erratum in: JAMA Netw Open. 2020 Jul 1;3(7):e2016899. PMID: 32614424; PMCID: PMC7333022.
241. Australian Resuscitation Council. Standards for Resuscitation: Clinical Practice and Education. 2014. Available from: http://resusorgau/standards-for-resuscitation-clinical-practice-and-education-release/. Accessed 01 May 2015.
242. Sherren P.B., Tricklebank S., Glover G. Development of a standard operating procedure and checklist for rapid sequence induction in the critically ill. Scand J Trauma Resusc Emerg Med. 2014 Sep 11;22:41. doi: 10.1186/s13049-014-0041-7. PMID: 25209044; PMCID: PMC4172951.
243. Sillén A. Cognitive tool for dealing with unexpected difficult airway. Br J Anaesth. 2014 Apr;112(4):773-4. doi: 10.1093/bja/aeu085. PMID: 24645169.
244. Goldhaber-Fiebert S.N., Howard S.K. Implementing emergency manuals: can cognitive aids help translate best practices for patient care during acute events? Anesth Analg. 2013 Nov;117(5):1149-61. doi: 10.1213/ANE.0b013e318298867a. PMID: 24108251.
245. Chrimes N.C. The Vortex: striving for simplicity, context independence and teamwork in an airway cognitive tool. Br J Anaesth. 2015 Jul;115(1):148-9. doi: 10.1093/bja/aev047. PMID: 26089469.
246. Duggan L.V., Brindley P.G. & Law J.A. Improving communication, teamwork, and action during a “cannot intubate cannot oxygenate (CICO)” emergency: employing CICO as a cognitive aid mnemonic. Can J Anesth/J Can Anesth 65, 1087–1092 (2018). https://doi.org/10.1007/s12630-018-1193-0.
247. Marshall S.D., Mehra R. The effects of a displayed cognitive aid on non-technical skills in a simulated 'can't intubate, can't oxygenate' crisis. Anaesthesia. 2014 Jul;69(7):669-77. doi: 10.1111/anae.12601. PMID: 24917333.
248. Harvey R., Foulds L., Housden T., Bennett K.A., Falzon D., McNarry A.F., Graham C.: The impact of didactic read-aloud action cards on the performance of cannula cricothyroidotomy in a simulated “can’t intubate can’t oxygenate” scenario. Anaesthesia 2017; 72:343–9.
249. Simmons W.R., Huang J. Operating Room Emergency Manuals Improve Patient Safety: A Systemic Review. Cureus. 2019 Jun 12;11(6):e4888. doi: 10.7759/cureus.4888. PMID: 31423368; PMCID: PMC6689479.
250. Huang J., Hoang P., Simmons W.R., Zhang J. Free Emergency Manual Books Improve Actual Clinical Use During Crisis in China. Cureus. 2019 Jun 3;11(6):e4821. doi: 10.7759/cureus.4821. PMID: 31403011; PMCID: PMC6682387.
251. Huang J., Wu J., Dai C., Zhang X., Ju H., Chen Y., Zhang C., Ye F., Tan Y., Zong Y., Liu T. Use of Emergency Manuals During Actual Critical Events in China: A Multi-Institutional Study. Simul Healthc. 2018 Aug;13(4):253-260. doi: 10.1097/SIH.0000000000000303. PMID: 29771811.
252. Ahmad I., El-Boghdadly K., Bhagrath R., Hodzovic I., McNarry A.F., Mir F., O'Sullivan E.P., Patel A., Stacey M., Vaughan D. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020 Apr;75(4):509-528. doi: 10.1111/anae.14904. Epub 2019 Nov 14. PMID: 31729018; PMCID: PMC7078877.
253. Xue F.S., Li C.W., Zhang G.H., et al. GlideScope-assisted awake fibreoptic intubation: initial experience in 13 patients. Anaesthesia. 2006;61(10): 1014-1015.
254. Greib N., Stojeba N., Dow W.A., Henderson J., Diemunsch P.A. A combined rigid videolaryngoscopy-flexible fibrescopy intubation technique under general anesthesia. Can J Anaesth. 2007;54(6):492-493.
255. Sahay N., Kumer R., Naaz S., Vivekanand. Awake supraglottic airway guided intubation: for the patient, by the patient. Korean J Anesthesiol. 2020 Jun;73(3):262-263. doi: 10.4097/kja.20055. Epub 2020 Apr 7. PMID: 32252515; PMCID: PMC7280893.
256. Bhalotra A.R. Awake supraglottic airway guided flexible bronchoscopic intubation. Korean J Anesthesiol. 2020 Apr;73(2):173-174. doi: 10.4097/kja.20013. Epub 2020 Jan 31. PMID: 32008276; PMCID: PMC7113161.
257. Lim W.Y., Wong P. Awake supraglottic airway guided flexible bronchoscopic intubation in patients with anticipated difficult airways: a case series and narrative review. Korean J Anesthesiol. 2019;72:548–57.
258. Hanna S.F., Mikat-Stevens M., Loo J., Uppal R., Jellish W.S., Adams M. Awake tracheal intubation in anticipated difficult airways: LMA Fastrach vs flexible bronchoscope: A pilot study. J Clin Anesth. 2017 Feb;37:31-37. doi: 10.1016/j.jclinane.2016.10.040. Epub 2016 Dec 22. PMID: 28235524.
259. Hodzovic I., Janakiraman C., Sudhir G., Goodwin N., Wilkes A.R., Latto I.P. Fibreoptic intubation through the laryngeal mask airway: effect of operator experience*. Anaesthesia. 2009;64:1066–71.
260. Asai T., Eguchi Y., Murao K., Niitsu T., Shingu K. Intubating laryngeal mask for fibreoptic intubation–particularly useful during neck stabilization. Can J Anaesth 2000; 47:

Таксономические единицы (категории) растений: Каждая система классификации состоит из определённых соподчиненных друг другу...
Состав сооружений: решетки и песколовки: Решетки – это первое устройство в схеме очистных сооружений. Они представляют...
Типы сооружений для обработки осадков: Септиками называются сооружения, в которых одновременно происходят осветление сточной жидкости...
Механическое удерживание земляных масс: Механическое удерживание земляных масс на склоне обеспечивают контрфорсными сооружениями различных конструкций...
© cyberpedia.su 2017-2024 - Не является автором материалов. Исключительное право сохранено за автором текста.
Если вы не хотите, чтобы данный материал был у нас на сайте, перейдите по ссылке: Нарушение авторских прав. Мы поможем в написании вашей работы!