
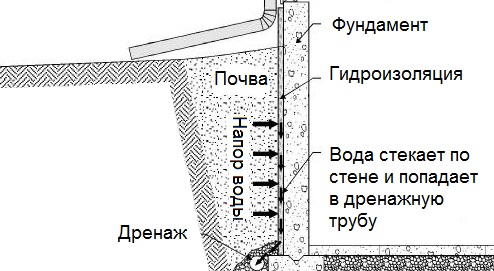
Общие условия выбора системы дренажа: Система дренажа выбирается в зависимости от характера защищаемого...
Биохимия спиртового брожения: Основу технологии получения пива составляет спиртовое брожение, - при котором сахар превращается...
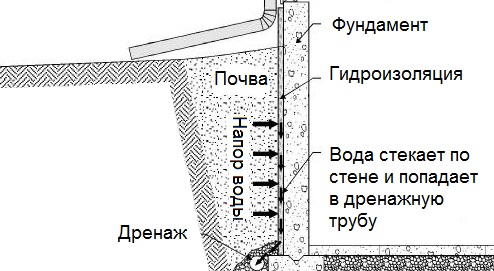
Общие условия выбора системы дренажа: Система дренажа выбирается в зависимости от характера защищаемого...
Биохимия спиртового брожения: Основу технологии получения пива составляет спиртовое брожение, - при котором сахар превращается...
Топ:
История развития методов оптимизации: теорема Куна-Таккера, метод Лагранжа, роль выпуклости в оптимизации...
Марксистская теория происхождения государства: По мнению Маркса и Энгельса, в основе развития общества, происходящих в нем изменений лежит...
Эволюция кровеносной системы позвоночных животных: Биологическая эволюция – необратимый процесс исторического развития живой природы...
Интересное:
Наиболее распространенные виды рака: Раковая опухоль — это самостоятельное новообразование, которое может возникнуть и от повышенного давления...
Лечение прогрессирующих форм рака: Одним из наиболее важных достижений экспериментальной химиотерапии опухолей, начатой в 60-х и реализованной в 70-х годах, является...
Финансовый рынок и его значение в управлении денежными потоками на современном этапе: любому предприятию для расширения производства и увеличения прибыли нужны...
Дисциплины:
|
из
5.00
|
Заказать работу |
|
|
|
|
CASE HISTORY/MEDICAL DOCUMENTATION
Составители: старшие преподаватели кафедры иностранных языков Санкт-Петербургской Государственной Педиатрической Медицинской Академии И.Л.Гальфанович, М.Ю.Дайнеко, Н.А.Мордвинова.
Рецензент: доцент кафедры романской филологии факультета иностранных языков РГПУ им. А.И.Герцена, кандидат педагогических наук В.Д.Макаричева.
Ответственный редактор: заведующая кафедрой иностранных языков Санкт-Петербургской Государственной Педиатрической Медицинской Академии, кандидат филологических наук доцент И.И.Могилёва.
Учебное пособие “Case History/Medical Documentation” предназначено для работы по подготовке студентов разных медицинских специальностей в рамках элективного курса, посвящённого паспортизации пациента.
Данное пособие имеет чёткую направленность на формирование навыков самостоятельной работы аудиторного и внеаудиторного планов и способствует выработке у студентов навыков классификации, анализа и синтеза, логически осмысленного чтения, выделения ключевых моментов в описании клинических случаев.
Учебное пособие состоит из 10 мини-модулей, содержащих задания по различным частям основного документа пациента – карте больного. Упражнения представляют собой вариативный материал – от элементарного заполнения бланков до креативной работы по самостоятельному созданию истории заболевания на основе информации по клинической картине. Структура пособия подразумевает последовательность комплексности, что позволяет использовать его при работе со студентами с разноуровневой подготовкой по программе школьного курса.
Dear medical student!
You are starting a medical career. You are going to become a doctor. There is a great variety of areas of medicine you can later choose. But whatever branch of medicine you will take, you will have to deal with medical documentation, fill in lots of special forms. The wide open world you live in will make you need to take part in international scientific or doctors’ conferences and meetings, to discuss current medical problems with foreign doctors or patients asking for your help. Three English languages of medicine will be necessary for you to do it, they are: the language medical professionals speak to each other, the language of their talks with patients and the language of medical documents. Medical documentation is written with abbreviations, letters and shortened word forms which every doctor understands. This book will help you to master the basics of the three medical English languages, the language of English medical documentation in particular, and to translate to and from these languages.
|
|
II.Taking Medical History
Choose the most suitable phrases for the situations below using the specialized Questionnaire and List of Commands (add your own variants if it is necessary):
1) You are questioning a patient on the state of his health. Find out:
A) the passport data, age, occupation, place of residence, marital status;
B) his complaints;
C) the onset of the disease.
2) You are taking the past history of your patient. You must know:
A) the diseases the patient had in his childhood;
B) if the patient was ill with TB (VD, AIDS);
C) if the patient has been operated on before;
D) if the patient consulted a doctor on his disease;
E) if a similar disease runs in the family.
3) You are questioning a patient on the signs and symptoms of the present illness. Try to find out:
A) the character of the onset of the pains (symptoms);
B) localization and character of the pain (symptom);
C) duration of the disease;
D) progress of the disease;
E) the factors aggravating the condition.
4) You are examining a patient with heart trouble. What do you say if:
A) you are listening to his heart;
B) you are listening to his lungs;
C) you are going to palpate (auscultate) him;
D) you are going to take his temperature;
E) you are going to measure his blood pressure.
5) You are examining a patient with an ulcer disease. Question him:
A) on the location of the pain;
B) on the character of the pain;
C) on the last fit of pains;
D) give your instructions to the patient how to prepare for the X-ray examination (roentgenoscopy) of the stomach.
Questionnaire
- What do you do?
- What’s your problem?
- Where do you feel the pain?
- Do the pains subside after applying a hot-water bottle?
- How long have you been ill?
- Have you ever been seriously ill?
- Do you have any belching? Is it of a sour or bitter taste?
- How old are you?
- What’s your job?
- Do you have any pains on an empty stomach?
- What diseases have you had in the past?
- When do the pains come on? Do they appear after meals?
- What’s your address, please?
- Have you been exposed to any industrial hazards at your place of work? Which ones?
- How long after meals do the pains begin?
- At what age did you begin working?
- Are you allergic to any drugs?
- Are there any night pains?
- What relieves the pains?
- Is your appetite good?
- Is there any burning sensation in the stomach? When do you feel it?
- Does nausea trouble you? How often? When?
- When did you vomit?
- When did the first symptoms appear?
|
|
- What’s your occupation?
- How many times a day do you have stools?
- Do you take laxatives? Are you given an enema?
- Do you have constipation or diarrhea?
- Has anybody in your family had tuberculosis (cancer, heart diseases, bronchial asthma, epilepsy, alcoholism)?
- What has brought you here?
- Do you have any pain in the heart region?
- Do you have a heart trouble?
- Have you ever been in hospital, if yes, for what reasons?
- Do you have a pain in the joints?
- Have you ever suffered from some heart trouble like this before?
- When and in what hospital were you treated?
- Did the disease recur from time to time?
- Have you consulted any doctor about this disease?
- Have you had your ECG made?
- Have you noticed any swelling?
- Have you ever been treated in a surgical department?
- When did this swelling appear?
- Do you always feel short of breath or does the breathlessness come from time to time, or at a certain time?
- What drugs relieve a fit of pain?
- Are you married or single?
- What diseases did you have in your childhood?
List of Commands
- Show where the pain is the most acute.
- Lie down flat on your back.
- Show me your tongue.
- Watch my finger.
- Let me look into your throat.
- Bend your body forward.
- Say ah.
- Undress, please.
- Strip to the waist.
- Turn your head and breathe.
- Breathe deeply.
- Breathe normally.
- Take a deep breath in and keep it.
- Dress up, please.
- Slip off your coat, please.
III.Medical Examination
Choose the proper set of questions (from part B) for the following points (from part A):
Part A:
1) Identification
2) CC (Chief Complaints)
3) HPI (History of Present Illness)
4) PH (Past History)
5) FH (Family History)
6) √ (Diagnosis)
Part B (I):
1) - What is the problem?
- I have difficulty in breathing, especially at night. You know, it constantly keeps me awake. I quite often have episodes of wheezing. The shortness of breath comes more and more frequently.
2) - Are you married?
- Yes.
- Have you got any children?
- No.
- Are your parents alive?
- Yes. They are healthy.
- And what about your grandparents?
- They died of heart failure when they were elderly.
- Your uncles and aunts?
- In good health.
- Have you ever heard your relatives talk about asthma in your family?
- No, never.
3) – Your diagnosis is bronchial asthma. It is a very serious disease. I advise you a change of climate, first of all.
4) – Who are you?
- Ann Brag.
- How old are you?
- 26 years old.
- What’s your address, please?
- 32, Forest Street, Eastpoint, Missouri.
5) – What diseases did you have in your childhood?
- Measles, mumps, chicken-pox.
- Any surgery?
- No, doctor.
- Will you tell me more details about your present illness?
- Yes, of course, I started having wheezing when I was 5. My parents told me that I had had shortness of breath after attacks of children diseases.
6) – When do you think the disease began? How long has it been troubling you?
- I was taken ill when I was 5 years old. Our family doctor advised my parents to take me to the sea for a change of air.
- How did you feel there?
- Fine. I had no trouble while staying at the sea. But when we returned home my breathing ailment recurred. I don’t feel well in cold and rainy weather.
- What treatment did your physician prescribe you?
- Inhalations. But my condition became worse, more severe. You know, tobacco smoke irritates me badly. My husband is a heavy smoker.
- Oh, my dear, you need only pure fresh air. He should know this.
Part B (II):
1) - Are you married?
- Yes.
- Do you have any children?
- Yes, two boys and a girl.
- Do you have any close relatives living?
- Yes, my parents and a brother are alive and healthy.
2) – What’s your name?
- __________ (fill in the gap)
- How old are you?
- __________ (fill in the gap)
- Where do you live?
- __________ (fill in the gap)
- What’s your occupation?
- __________ (fill in the gap)
|
|
3) – What diseases have you had?
- Whooping cough, mumps, measles.
- Have you ever had pneumonia or kidney trouble?
- I often caught colds in winter and had pneumonia, that’s all I remember.
- Any harmful habits?
- I neither smoke nor drink.
4) – What’s your trouble?
- I have persistent coughing and pains in the chest.
5) – I suspect you have pneumonia as a complication after influenza. But to confirm the diagnosis you have to have your tests of blood, urine and X-ray examination made.
6) – When did you notice the first signs of the disease?
- I had influenza a week ago, but I followed the doctor’s recommendations and recovered rather quickly.
- When did you feel chest pain for the first time?
- Two days later.
- Can you relieve it by any drug?
- No.
- Do you cough up any phlegm?
- Yes, a little.
Part B (III):
1) - Are you married?
- Yes, but we are childless.
- Do you have parents? Are they well?
- My mother died of diabetes, my father of heart trouble.
- Have you any sisters or brothers?
- No, I have no relatives.
2) – Have you ever been sick?
- In childhood I had some children diseases but I don’t remember which of them.
- Have you ever been operated on?
- Five years ago I had urethral resection made.
- Any bad after-effects of the surgery?
- No, not any.
- Did you seek medical attention to clear the cause of your trouble?
- Yes, my family doctor advised me some drugs and to have a good rest, but with no effect.
3) – What’s your opinion, are these epileptic attacks?
- No, I’m sure you have been suffering from heart trouble for a rather long time. Your seizures have been connected with cardiac standstill. It is difficult to manage. I think of installing a pacemaker, with your coming for check-ups yearly.
4) – What problem do you have?
- I have been having a feeling of heaviness in my chest for more than a year.
- Any pain?
- Not any, Doctor, but three or four times when I was gardening, I had recurrent episodes of convulsions, brief seizures.
- Do you have headaches?
- No, not often.
- Do you feel worried or nervous?
5) – What’s your name?
- I’m Mrs. Gross.
- How old are you?
- I’m 50, doctor.
- Your address?
- 38, Rockland Road.
- What do you do for living?
- I’m a housewife, I have a large family.
6) – A feeling of heaviness in the chest, convulsions, tiredness, seizures, loss of consciousness.
V.Medical Kits
Compose a suitable medical emergency kit for:
A) home;
B) car;
C) travel.
(Some items may be used for different kits)
(Add some individually required remedies!)
| Sterile gauze dressing Cotton applicators Thermometer Aspirin Iodine Petroleum jelly Distilled water Rubbing alcohol Cough syrup Cups Splint Honey Activated charcoal Paracetamol Salt Baking soda Hemostyptic pencil Painkillers Pair of scissors Medical gloves Eye drops Adhesive plaster Mustard plaster Brilliant green solution Manganese crystals Disposable syringes Pump oxygenator Blood pressure measurement apparatus Enema syringe Purgative medicine Antiemetic medicine Hematogen Vitamin C Bandage Earplugs Cloth tourniquet Validol Nasal drops |
VI.Reading Medicine Labels
Match A and B to understand the information medicine labels contain:
1)
| A | B |
| KORPEX Relieves coughs, fever, headaches Aspirin, coriniol, hexaperon Wonder Drugs, USA 2 tablets every 3 hours KORPEX tablets can be chewed or swallowed No more than 10 tablets daily over a 1-week period Not advisable for pregnant women May cause drowsiness | · How to take a dose · Name of the product · Possible side effects · Total dose that may be taken a day · Active ingredients · The amount of each dose · Symptoms the product relieves · Limitation · Company producing the product · Frequency with which it may be taken |
2)
|
|
| A | B |
| Apply 1-2 times daily, continuing for 2-3 weeks after lesions have healed Occasional local irritation and hypersensitivity reactions include mild burning sensation, erythema, and itching, rare blistering; treatment should be discontinued if these are severe Fungal skin infections SULKANAZOLE NITRATE Extraderm, Hungary Contact with eyes and mucous membranes should be avoided | · Side-effects · Name of the product · Dose · Company producing the medicine · Cautions · Indications |
3)
| A | B |
| Anti-viral throat spray as a part of complex therapy ANAFERON KID SPRAY No registed cases of overdosage Is not used for infants under 1 month The recommended scheme requires 3-5 times a day usage Interferon gamma antibodies White colour can (contains colourless liquid with pleasant smell) with a special spray tube “MateriaMedCompany”, Moscow, Russia | · Name of the product · Active ingredients · Company producing the medicine · Indications for usage · Recommendations on limitation · Description of the product · Possible reactions in the case of overdosage · How often to use the spray |
Think up a medicine label of a drug used for the treatment of:
A) Heart failure;
B) Diarrhea;
C) Headaches.
IX.Medical Record
Read the dialogue between Doctor Johnson and a medical student through. Then read and translate the first case below. Using the sections of the medical record Dr. Johnson is reading in the dialogue as a model, fill in the similar sections for Case 1. Continue making up medical records with the same sections for the other cases described.
The diagnoses of these cases are given after the 7th Case. You are not qualified enough yet to find the correct diagnosis to each case. However, you could try, think and guess, relying on some medical knowledge you do have. Prepare to give your reasons why you have chosen the particular diagnosis. Your lecturer will give you the correct diagnosis of the doctors.
Dr.Johnson: So, what is the history of your new case? Let me see it!
Medical Student: Here you are!
Dr.Johnson (reads):
Patient: Paul Brown.
Age: 58.
Sex: Male.
Occupation: Engineer.
Family status: Married.
Family history: Wife and four children living and well; father living and well; mother died: the result of a street accident; two sisters and а brother living and well.
Past history: Measles, scarlet fever and pneumonia in childhood; two ribs fractured: the result of a war wound; neither drinks nor smokes.
Present complaints: A severe pain in the abdomen (the right iliac region); nausea and vomiting; temperature 39ºC.
Duration: 2 days.
Diagnosis: Acute appendicitis.
Dr.Johnson: In most cases, appendicitis is not difficult to diagnose, but sometimes the picture is that of acute intestinal process, e.g. enterocolitis. It is particularly easy to overlook it in children, in whom its course is a violent one and often produces general phenomena with negligible local ones. Children cannot point out the location of pain and often complain of it in the epigastrium or all over the abdomen. Tell me, please, what does his physical examination reveal?
Medical Student: The physical examination of my patient reveals pain and limited muscular tension in the right iliac region. The clinical picture is the one of acute appendicitis.
Dr.Johnson: I agree with you that his symptoms are those of acute appendicitis.
VOCABULARY OF MEDICAL TERMS TO THE CASE REPORTS:
productive cough влажный кашель
sputum=phlegm мокрота
on exertion=on effort при напряжении
cyanotic blush цианотический румянец
heart sound сердечный тон
clapping sound хлопающий тон сердца
dull sound притупленный, глухой тон
presystolic murmur пресистолический шум
pleural fremitus =rub шум трения плевры
exposure to cold пребывание на холоде
expose to cold подвергать воздействию холода
pulse of an average fullness пульс среднего наполнения
regular shape правильная форма
it is somewhat retarded она несколько отстает
harsh breathing (respiration) жесткое дыхание
amphoric breathing амфорическое дыхание
tympanitic resonance тимпанический звук
loss of resonance притупление перкуторного звука
infiltrate darkening инфильтративное затемнение
|
|
erythrocyte sedimentation rate (ESR) СОЭ (скорость оседания эритроцитов)
shift to the left сдвиг влево
vocal fremitus голосовое дрожание
forced position вынужденное положение
injected veins набухшие вены
the border is moved down граница опущена
mobility подвижность
disseminated rales рассеянные хрипы
moist rales влажные хрипы
sonorous coarse rales звучные крупные хрипы
medium bubbling rales средне-пузырчатые хрипы
single rales единичные хрипы
median line средняя линия
from the medioclavicular line out снаружи от средне-ключичной линии
fall into layers распадаться на слои
accent акцент
accentuated акцентуированный
interscapular space межлопаточное пространство
dyspnea одышка
compressing pain сжимающая боль
edema отек
hypochondrium подреберье
vascular wall сосудистая стенка
outside the pulse wave вне пульсовой волны
spread heart beat разлитой сердечный толчок
CASE 1
The doctor was called in as the patient, Eric Someson, complained of high temperature, pains in the right side on deep respiration, dry cough. The onset was sudden, the day before while working he felt malaise, chill, a slight cough appeared. In the evening the temperature was 38ºC, today in the morning it was 38,4ºC. He had never had anything like this illness before. He had suffered from measles, quinsies, now and again an upper respiratory infection. The patient is 38, male, works as a driver. He believes his illness is due to his exposure to cold.
Objective findings: there is feverish blush on his face, his position is active. The pulse rate is 90 per minute, rhythmic, of an average fullness and tension. His heart borders and sounds are normal. The shape of his chest is regular, the right side of it is somewhat retarded in breathing, respiration rate is 18 per minute. On percussion a dull sound (loss of resonance) was revealed in the right subscapular area. There is slightly harsh breathing and pleural rub in the same area.
CASE 2
Mike Green was brought to the in-patient department as an emergency case with complaints of fever, the temperature being up to 38,5-39ºC, pains in the left side of the chest, especially bad on respiration, cough with a small amount of mucopurulent sputum without any smell. The patient had been ill for a week. The onset had been sudden, the temperature rising to 38ºC, with cough and pains in the left side. He had been on a business trip at the time, and because of this he hadn’t consulted a doctor. Having returned home he called in the doctor who insisted on hospitalization.
The patient is 41, male, works as an engineer at a plant. He believes the cause of his illness to be his exposure to cold. He had hardly any complaints in the past, only once in a while he had an upper respiratory infection or quinsy.
Objective findings: the patient’s general condition is bad, there is feverish blush, dyspnea, superficial breathing, respiration rate is 24 per minute. The pulse rate is 120 per minute, it is small, soft. Blood pressure is 100 over 60 mm. The heart borders are normal, the first sound is slightly dull. The chest on the left is retarded on respiration. On the left at the back the lung border cannot be determined, on the right the lung border is normal. There is a pleural friction rub along the lower side. The vocal fremitus and bronchophony are increased.
CASE 3
Evan Wilson, aged 50, male, was brought to the in-patient department as a case of emergency. He complained of a pain in the right side of his chest which set in abruptly and of short breath. He had been ill with an upper respiratory infection for some days when an acute pain in his side and breathlessness developed on a bad attack of coughing. The temperature is normal. The patient used to suffer from bronchitis in the past, he smokes.
Objective findings: the patient’s general condition is of an average severity, he takes a forced sitting position, respiration rate is 28 per minute, he is pale, his lips are cyanotic, the veins on his neck are injected, the right side of his chest doesn’t take part in the respiration. The breathing is absent over the right side of the chest, over the left side dry rales are heard. Pulse rate is 90 per minute.
CASE 4
The patient, Peter Smith, aged 38, male, has been staying in the in-patient department for 3 weeks. At present he complains of subfebrile temperature, cough with a large amount of sputum (200 gr per day), having a foul smell (if kept it falls into layers), mild pains in the right side of his chest. He had felt ill for a month before, when subfebrile temperature, dry cough and cold in the head appeared. The patient continued working for a week, but then his temperature rose up to 38-39ºC and he was hospitalized. A week ago expectoration of a large amount of purulent sputum developed, his temperature dropped and became subfebrile, his condition somewhat improved.
The patient works as a shopmaster at a factory, he is often exposed to draughts at his shop and frequently catches cold, he had pneumonia twice. He smokes, drinks alcohol regularly, almost daily. He believes his illness is due to his having been exposed to severe cold when drunk.
Objective findings: general condition of the patient is rather severe. The position is active, but he tends to lie on the right side as cough worries him less in this position. The patient is grayish-pale, his pulse is frequent, pulse rate is 90 per minute, heart borders are within the normal limits, the first heart sound is somewhat weakened, the second one is accentuated on the pulmonary artery.
CASE 5
Jane Melton is 55, female, she was admitted to the in-patient department with the complaints of subfebrile temperature, persistent cough with a small amount of mucopurulent sputum without any smell, a bad general weakness, sweating, a feeling of heaviness and pains in the right side of her chest, especially on deep respiration. She fell ill two weeks ago when cold in the head and malaise appeared. Her temperature was normal, so she continued working. A week later her cough increased, a small amount of sputum appeared, the temperature began to rise. Then the patient was given a sick leave and treated by an expectorating mixture, mustard plasters, aspirin. As her condition didn’t improve, the doctor referred her to the hospital.
Objective findings: the patient’s general condition is not bad, there is no dyspnea. Her pulse is rhythmic, of an average fullness and tension, pulse rate is 86 per minute. Heart borders and sounds are within the normal limits. The chest mobility is normal, there is no retardation in breathing. On percussion the lung borders were found to be normal, on the right there was noticed limited mobility of the lung border along the back surface, loss of resonance in the right intrascapular space, one could hear harsh breathing and fine bubbling moist rales, sonorous ones.
CASE 6
Catherine Reice, aged 30, female, complains of breathlessness, productive cough with expectoration of a small amount of sputum, occasionally bloody. When a child, she used to suffer from quinsies. She had tonsillectomy at 12. Dyspnea first developed two years ago. Breathlessness increased and expectoration of bloody sputum appeared a few days ago on physical exertion.
Objective findings: she has cyanotic blush on her cheeks, her pulse rate is 120 per minute, small, rhythmic. In the cardiac region the heart beat is displaced to the right, which is confirmed by palpation. The heart borders are dilated upwards and to the right, the first sound is clapping, the second sound accent is on the pulmonary artery, there is a presystolic murmur at the apex.
CASE 7
Alan Gray, 67, male, complains of compressing pains in the cardiac area, radiating to the left shoulder, arm, to the region of the 4th-5th finger. The pains are associated with physical exertion and excitement. In addition the patient complains of dyspnea, edema of his feet developing towards night, feeling of heaviness in the right hypochondrium. He has been suffering from pains in the heart area for 10 years, with nitroglycerin relieving them. The pains occurred seldom at first and he was treated as an out-patient. He considers his last setback to be associated with overwork due to an urgent problem at his shop. He works as a senior master at a factory. In the past he had rare colds, smoked much. He drinks alcohol regularly.
Objective findings: he has acrocyanosis, the pulse rate is 106 per minute, rhythmic, of an average fullness, hard. The vascular wall may be palpated outside the pulse wave. The spread heart beat is auscultated in the 5th intercostal space, 2-3 cm from the mediaclavicular line out, on the left. His heart borders are extended to the left, 2 cm from the left mediaclavicular line. The first heart sound is weakened and dull, the second one is accentuated on the aorta. Systolic murmur is heard at the heart apex. Blood pressure is 160 over 70 mm Hg. In the lungs single, moist rales, with somewhat harsh breathing at the background, are heard in the posterobasal parts. The abdomen is soft, tender, the liver edge is palpated 2-3 cm under the ribs, it is round, soft, tender.
DIAGNOSES
The cases above describe:
right pneumothorax associated with an acute attack of chronic bronchitis;
coronary vascular angina pectoris(stenocardia) with mitral and circulatory insufficiency and cadiosclerosis;
right focal pneumonia of the lower lobe;
lung abcess;
croupous pneumonia;
dry pleurisy associated with pneumonia;
mitral stenosis associated with the left ventricular circulatory failure.
X.Problem Solving
Each of the numbered items in this section is followed by possible answers. Try to select the one lettered answer or completion that is best in each case, discuss it with your partner(s) and comment on your choice trying to prove your decision:
1) An 8-year-old boy with acute lymphoblastic leukemia has had three relapses over the past 2 years. The only available treatment is experimental chemotherapy. Without treatment, the child is unlikely to survive for more than 6 weeks; with treatment his prognosis is unknown. The parents do not want further treatment for their son and wish to take him home; the child also says he wants to go home. Which of the following is the most appropriate course of action?
A) Discharge the child against medical advice;
B) Discharge the child routinely;
C) Petition the court for an order for treatment;
D) Report of the parents to the child protective services for medical neglect.
2) A nurse is hospitalized for appendectomy at the medical center where she is employed. One week after discharge, the assistant hospital administrator asks the surgeon who performed the procedure about the final diagnosis. Which of the following is the most appropriate response on the part of the surgeon?
A) Answer, because it will expedite handling of insurance issues at the medical center;
B) Answer, because as an employee of the medical center the administrator has access to information about patients;
C) Answer, because of the possibility of spreading misinformation about the patient;
D) Decline to answer, because the administrator is not a medical doctor;
E) Decline to answer, because the information is confidential.
3) An asymptomatic 3-year-old boy is brought to the physician for a routine examination. Small, inguinal lymph nodes are palpable; no other abnormalities are noted. Which of the following is the most appropriate next step?
A) Schedule a routine follow-up examination;
B) Urine culture for bacteria;
C) Tape test for pinworms;
D) Monospot test;
E) Complete blood test.
4) A 10-month-old girl, who happily allowed herself to be held when her grandmother visited 2 months ago, now cries when her mother tries to put her in her grandmother’s arms. The most likely explanation is that the child has
A) Been maltreated by the grandmother;
B) Begun to develop problem with socialization;
C) Normal stranger anxiety;
D) A sense of poor relationship between the mother and the grandmother;
E) Separation anxiety disorder.
5) An 8-year-old boy needs to be coaxed to go to school and often, while there, complains of severe headaches or stomach pain. Sometimes his mother has to take him home because of his symptoms. At night, he tries to sleep with his parents. When they insist he sleeps in his room, he says there are monsters in his closet. This history is most consistent with
A) Childhood schizophrenia;
B) Normal concerns of latency-age children;
C) Separation anxiety disorder;
D) Socialized conduct disorder;
E) Symbiotic psychosis.
6) A 70-year-old widower has ecchymosys, perifollicular petechiae, and swelling of the gingival. His diet consists primarily of cola and hot dogs. The most likely diagnosis is
A) Beriberi;
B) Kwashiorkor;
C) Pellagra;
D) Rickets;
E) Scurvy.
7) A 12-year-old girl has incurable muscular dystrophy and has been in a persistent vegetable state for 5 years. Her parents are actually eager to take her to Switzerland to end her life as assisted dying is legal there. Opponents of euthanasia, or ‘mercy killing’, argue that legalization would lead to abuse and call for doctors who participate to be struck off. Those people who are against euthanasia suppose that Public Health Care Service has to organize better palliative care and more hospices for the terminally ill to allow such patients to die with dignity. Which of the following is true to the situation?
A) It’s not correct to continue the critically ill girl’s suffering;
B) You would agree to assist in the death of such a child to end the useless existence;
C) You are against the parents’ position;
D) You are constantly trying to find some experimental drug to help to improve the girl’s condition.
CLINICAL HISTORY 1
A 5 month-old male infant John McConnwale was brought to the Emergency Department by his parents with persistent, worsening shortness of breath and wheezing associated with excitement and physical exertion. The boy was lethargic, anorexic. He had a history of poor sleep and crying for two days. No fever, diarrhea, vomiting, foreign-body ingestion were noted. No asthma, recent illness or antibiotic ingestion, home treatment, recent infectious exposure or immunizations were recorded. There was evidence of dehydration, with limited tearing and decreased urine output. Oral intake was limited.
A chest Computed Tomography showed large, thin-walled cysts occupying most of the left hemithorax. A small portion of collapsed lung was present in the left upper thorax. The largest cyst was approximately 8 cm. There was a significant mass with mediastinal shift to the right. The right lung was essentially clear. There was no evidence of pneumothorax. The impression was of congenital cystic malformation of the lung.
CLINICAL HISTORY 2
A 21-year old Caroline Montley, student of Law University had 5 episodes of wheezing attacks during her childhood associated with mumps, chicken-pox, and common colds. After a move to the California coast at the age of 13, she had no asthmatic symptoms up to the present case. She is in distress, with labored breathing. The patient has a sensation of chest constriction. She produces coarse dry rales in the bronchial tubes. She thinks that continual wheezing and mild dyspnea are connected with relatively cold and damp months, at times with the periods of emotional upset, and after exposure to tobacco smoke. The symptoms are not aggravated by exposure to animal or house dust. The physical examination reveals increased resonance to percussion. Chest X-ray films show marked abnormalities.
CLINICAL HISTORY 3
A 2-year-old boy Jacob Witch was brought to the local General Practitioner by his mother. After the medical examination he was immediately referred to the city hospital. Five days before the admission he began to vomit and became irritable. He had a bad weakness, sweating and malaise.
On the admission a brain Computed Tomography was performed which revealed a large midline mass; the lesion was heterogeneous, cystic, partly solid with calcifications. Magnetic resonance imaging demonstrated a 5x4.9x4.7cm mass, extending into the left angle. The patient was operated upon and a total resection of the mass was performed.
CLINICAL HISTORY 4
A 34-year old school teacher of Geography Julia Mettew came to one of the clinics complaining of bad headaches and generalized malaise which lasted out. The temperature was 38,4º, the pulse rate 120, and the respiration 27 per minute. The throat was acutely inflamed and edematous and both tonsils were covered with an exudate. The patient was hospitalized and on the tenth day when the throat appeared normal and her ward doctor thought that the temperature should decrease too, it continued to be elevated and the woman complained that she could not swallow at all. A few hours later she refused to take the food. Local examination at this time revealed a swelling on the anterior surface of the neck above and in the region of the thyroid gland. The patient’s complaint that she could not swallow was confirmed by having her drink water under the observation: each time that she attempted to swallow it, the water came through her nose. A diagnosis of abscess of the prevertebral fascial space was made and the operation was performed. An incision, three and a half inches in length, was made. An aspirating needle was inserted into the mass and thick creamy pus was evacuated. The recovery was uneventful and the patient was discharged ten days later.
CLINICAL HISTORY 5
A 16 month old female Cristina Horthex was admitted to the Pediatric Intensive Care Unit with fever, hypoxia, altered mental status, breathlessness, and seizures. Magnetic resonance imaging (MRI) of the brain showed a single intraventricular mass which could be isolated easily because of dense cells concentration. The mass measured 4x4x4 cm. There was additional, but mild right lateral ventricular dilatation. These characteristics were most suggestive of a meningioma.
The patient subsequently had surgical resection of the mass with MRI Navigation Guidance. The mass had a thick capsule and a rubber like core. The tumor was removed without intraoperative complications. The patient was discharged home 4 days later and had done well since that time with no neurological disorders.
The child's parents underwent extensive genetic counseling and were encouraged to undergo mutation analysis as both are in their early twenties.
CLINICAL HISTORY 6
A pregnant woman Monica Lux, aged 19, had two spontaneous early abortions. On clinical grounds delivery was expected in the middle of February. The present pregnancy ran a normal course. On December 8, when the pregnancy was estimated to have lasted approximately 32 weeks, the patient was hospitalized for probable fetus growth retardation and mild vaginal blood loss. In spite of treatment and a salt-free diet the blood pressure rose up to 170 over 110 and the patient had constant sense of nausea. On December 12, 06.15.am, the patient had a few contractions, the base line of the fetal heart rate was 155 to 160 beats per minute. On December 13, 11.35.am, the fetal heart sounds could no longer be heard and a female dead fetus, weighing 1600 grams, 31 cm longer was delivered. There were no congenital abnormalities. The placental weight was 230 grams. There was noticed an important ischemic necrosis with vascular necrosis.
CLINICAL HISTORY 7
The patient is a 6-year old girl, Bernarda Crix, with past medical history significant for biliary cirrhosis. The patient, at one year of age, underwent a liver transplantation. This time she is admitted with an enlarging left neck nodal mass.
On admission significant laboratory findings include:
Hemoglobin-12.2g/dL;
Increased white blood cell count with:
Neutrophiles-49%,
Lymphocytes-31%,
Monocytes-9%,
Eosinophils-10%,
Basophils-1%.;
Renal function tests, electrolytes, glucose-within normal limits.
The examination reveals two partially affected practically equal in size lymph nodes matted together (4.5 x 2.5 x 1.5 cm).
CLINICAL HISTORY 8
A 45-year-old electrician Kent Renou fell 3 meters on January 5 and was unconscious for 15 minutes. He was found by his neighbours and wife and admitted to the hospital where after regaining consciousness, he complained of pain in both shoulders and neck and of numbness of the second and third fingers of the right hand. He was noted to have limitation of neck motion. A cervical spine roentgenogram, taken at the time of his admission, included only five upper vertebrae. A complete roentgenographic series of the cervical spine taken the next day was normal. He was treated by physiotherapy and discharged several days later.
His complaints persisted and two months later a consultation revealed a tilt of his head to the right, limitation and diffuse tenderness of the posterior neck muscles. The right triceps reflex was absent with hypoesthesia to pin prick over the second and third fingers of the right hand. A lateral cervical X-ray film demonstrated a first-degree delayed traumatic dislocation of the cervical spine. An anterior cervical disk-ectomy and reduction of the cervical vertebrae were performed. The patient did well and was asymptomatic ten months later with roentgenographic evidence.
CLINICAL HISTORY 9
A 3-year-old girl Marisha Pishka with a history of mild motor delay was presented with a change in mental status, gait difficulties, nausea and vomiting. The patient was in her usual state of health until 9 months prior to presentation, when she was found to have abnormalities of the left eye. Over the next several months, she developed gait difficulties and behavioral changes. On the day of admission, she developed confusion, severe gait difficulties, nausea and profuse vomiting. On physical examination, she had increased deep tendon reflexes of her right Achilles tendon. She subsequently became unresponsive. She was intubated and given mannitol and steroids. An external ventricular drain was placed. Neuroimaging showed a minimally heterogeneous tumor measuring 8×8×9 cm involving the left parietal region and, partly filling the left lateral ventricle. Gross total resection of the tumor was confirmed by post-operative imaging. Staging evaluation revealed no metastasis. The patient was discharged one week later.
CLINICAL HISTORY 10
The patient Robert Bush was born at 38 weeks via C-section. The pregnancy was complicated by gestational diabetes in the mother who was treated. She also had elevated liver function tests (LFTs) during pregnancy; otherwise, no additional problems were noted. He was 7 pounds 14 ounces. The patient was diagnosed with neonatal jaundice, treated with phototherapy and discharged three days after birth.
This baby boy with postnatal onset microcephaly had speech impairment and global developmental delay that were noted at 12 months of age. He also had feeding problems which included gagging, choking and frequent drooling. The mother also noted that the child has been sleeping more in recent weeks. According to the mother, the infrequent episodes are typified by the boy stopping suddenly, staring and becoming unresponsive. The child's history is negative for convulsions, meningitis, encephalitis or severe head trauma associated with loss of consciousness. There is no family history of developmental delay or neurological problems. The boy is characterized by frequent smiling and laughter, hyperactivity. He has a strikingly pale hair and unusually pale blue eyes. Involuntary hand movements, wide-based gait, and dystonically upgoing toes are noticed. The patient's physical examination is positive. An EEG was performed and showed a normal awake-and-asleep pattern; however, a subtle slow background frequency for age was noted. An MRI was positive. A blood sample from the patient was sent for DNA molecular testing.
CASE HISTORY/MEDICAL DOCUMENTATION
Составители: старшие преподаватели кафедры иностранных языков Санкт-Петербургской Государственной Педиатрической Медицинской Академии И.Л.Гальфанович, М.Ю.Дайнеко, Н.А.Мордвинова.
Рецензент: доцент кафедры романской филологии факультета иностранных языков РГПУ им. А.И.Герцена, кандидат педагогических наук В.Д.Макаричева.
Ответственный редактор: заведующая кафедрой иностранных языков Санкт-Петербургской Государственной Педиатрической Медицинской Академии, кандидат филологических наук доцент И.И.Могилёва.
Учебное пособие “Case History/Medical Documentation” предназначено для работы по подготовке студентов разных медицинских специальностей в рамках элективного курса, посвящённого паспортизации пациента.
Данное пособие имеет чёткую направленность на формирование навыков самостоятельной работы аудиторного и внеаудиторного планов и способствует выработке у студентов навыков классификации, анализа и синтеза, логически осмысленного чтения, выделения ключевых моментов в описании клинических случаев.
Учебное пособие состоит из 10 мини-модулей, содержащих задания по различным частям основного документа пациента – карте больного. Упражнения представляют собой вариативный материал – от элементарного заполнения бланков до креативной работы по самостоятельному созданию истории заболевания на основе информации по клинической картине. Структура пособия подразумевает последовательность комплексности, что позволяет использовать его при работе со студентами с разноуровневой подготовкой по программе школьного курса.
Dear medical student!
You are starting a medical career. You are going to become a doctor. There is a great variety of areas of medicine you can later choose. But whatever branch of medicine you will take, you will have to deal with medical documentation, fill in lots of special forms. The wide open world you live in will make you need to take part in international scientific or doctors’ conferences and meetings, to discuss current medical problems with foreign doctors or patients asking for your help. Three English languages of medicine will be necessary for you to do it, they are: the language medical professionals speak to each other, the language of their talks with patients and the language of medical documents. Medical documentation is written with abbreviations, letters and shortened word forms which every doctor understands. This book will help you to master the basics of the three medical English languages, the language of English medical documentation in particular, and to translate to and from these languages.
|
|
|
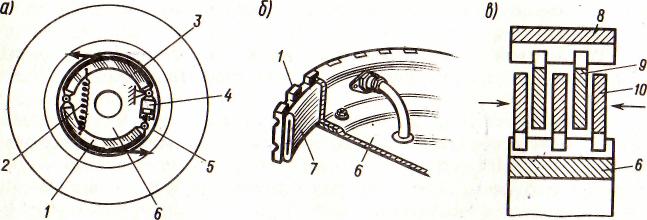
Автоматическое растормаживание колес: Тормозные устройства колес предназначены для уменьшения длины пробега и улучшения маневрирования ВС при...
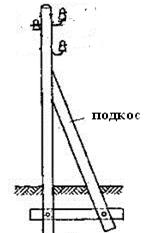
Опора деревянной одностоечной и способы укрепление угловых опор: Опоры ВЛ - конструкции, предназначенные для поддерживания проводов на необходимой высоте над землей, водой...
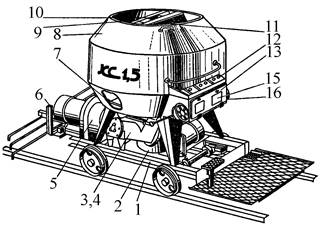
Кормораздатчик мобильный электрифицированный: схема и процесс работы устройства...
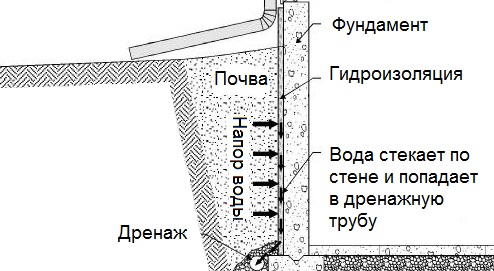
Общие условия выбора системы дренажа: Система дренажа выбирается в зависимости от характера защищаемого...
© cyberpedia.su 2017-2024 - Не является автором материалов. Исключительное право сохранено за автором текста.
Если вы не хотите, чтобы данный материал был у нас на сайте, перейдите по ссылке: Нарушение авторских прав. Мы поможем в написании вашей работы!