
Индивидуальные и групповые автопоилки: для животных. Схемы и конструкции...
Состав сооружений: решетки и песколовки: Решетки – это первое устройство в схеме очистных сооружений. Они представляют...
Индивидуальные и групповые автопоилки: для животных. Схемы и конструкции...
Состав сооружений: решетки и песколовки: Решетки – это первое устройство в схеме очистных сооружений. Они представляют...
Топ:
Марксистская теория происхождения государства: По мнению Маркса и Энгельса, в основе развития общества, происходящих в нем изменений лежит...
Определение места расположения распределительного центра: Фирма реализует продукцию на рынках сбыта и имеет постоянных поставщиков в разных регионах. Увеличение объема продаж...
Теоретическая значимость работы: Описание теоретической значимости (ценности) результатов исследования должно присутствовать во введении...
Интересное:
Национальное богатство страны и его составляющие: для оценки элементов национального богатства используются...
Уполаживание и террасирование склонов: Если глубина оврага более 5 м необходимо устройство берм. Варианты использования оврагов для градостроительных целей...
Искусственное повышение поверхности территории: Варианты искусственного повышения поверхности территории необходимо выбирать на основе анализа следующих характеристик защищаемой территории...
Дисциплины:
|
из
5.00
|
Заказать работу |
|
|
|
|
Популяция детей и взрослых с ВПС расширяется, и это – главный субстрат для ИЭ у молодых пациентов. Однако, наше знание ИЭ в этом окружении ограничено, так как систематических исследований немного и они часто ретроспективны, и смещение выбора, связанное с исследованиями узкоспециализированных центров,
препятсвует широкому применению.
Сообщаемая частота ИЭ при ВПС в 15-140 раз выше, чем в общей популяции (самое высокая оценка возникновения в узкоспециализированных отделениях).361,362 Сообщаемая пропорция ВПС у пациентов с ИЭ изменяется, вероятно из-за смещения выбора, между 2% и 18%,363–365 с постоянным незначительным преобладанием мужчин.58,362,366
Некоторые простые пороки, такой как дефект межпредсердной перегородки типа secundum и порок легочного клапана несут низкий риск ИЭ. Однако, ВПС часто состоит из нескольких сердечных повреждений, каждый из которых дополняет общий риск ИЭ. Например, частота ИЭ значительно выше у пациентов с дефектом межжелудочковой перегородки, когда ассоциированная аортальная регургитация.367
Распределение возбудителей не отличается от такового при приобретенных болезнях сердца, стрептококки и стафилококки являются самыми частыми штаммами.58,362,366
Основные симптомы, осложнения и основание для диагноза не отличаются от ИЭ в общем случае. Однако, правосторонний ИЭ является более частым при ВПС чем при приобретенной болезни сердца. Превосходство
ТЕЕ над TTE не было систематически изучено в этом окружении. Однако, сложная анатомия и присутствие искусственного материала могут уменьшить частоту обнаружения вегетаций и других особенностей ИЭ, таким образом одобряя дополнение ТЕЕ, особенно в группе взрослых.362 Однако, отрицательное исследование не исключает диагноз.
|
|
Лечение ИЭ при ВПС следует из общих принципов. Операция на сердце является соответствующей, когда медикаментозная терапия терпит неудачу, когда возникают тяжелые гемодинамические осложнения, и когда есть высокий риск разрушительной септической эмболии.
ИЭ при ВПС несет смертность 4-10%.58,62,362,366 Это лучший прогноз по сравнению с приобретенной болезнью сердца наводит на размышления о более высокой пропорции правосердечного ИЭ.
Первичное профилактика жизненно важна.368 Важность хорошей оральной, дентальной и кожной гигиены была уже подчеркнута, и антибиотическая профилактика обозначена в группах высокого риска, как определено в Разделе E. Однако, есть также образовательная проблема, и понимание риска ИЭ и потребность в профилактических мерах не удовлетворительно распространены в популяции с ВПС.369 Косметический персинг, по меньшей мере затрагивающий язык и слизистые, должен быть запрещен в этой группе.
Хирургическая пластика ВПС часто уменьшает риск ИЭ, если нет остаточных повреждений364,370 Однако, в других случаях, когда имплантирован искусственный клапан, процедура может увеличить общий риск ИЭ. Нет научных данных, оправдывающих сердечную операцию или чрезкожные вмешательства (например, закрытие открытого артериального протока) с единственной целью устранить риск ИЭ.371 Сердечная пластика как вторичная превентивная мера для уменьшения риска рецидива ИЭ была описана, но не была систематически изучена.
Таким образом, ИЭ при ВПС бывает редко и более часто затрагивает правое сердце. Сложная анатомия делает эхокардиографическую оценку трудной. Прогноз лучше чем при других формах ИЭ, со смертностью <10%. Профилактические меры и обучение пациентов имеют особое значение в этой популяции.
Часть 5. Инфекционный эндокардит у пожилых
ИЭ у пожилых (> 70 лет) является все более и более частым и ассоциируется с определенными особенностями.372 Относительная частота ИЭ, затрагивающего пожилых, была 26% в Euro Heart Survey,373 и 33% пациентов были старше 67 лет во Французском регистре.80 Во Французских обзорах частота ИЭ увеличилась между 1991 и 1999 годами среди пациентов > 50 лет и достиг максимума 145 случаев на миллион между 70 и 80-летним возрастом.14
|
|
Предыдущие сообщения показали, хотя не совсем убедительно, что ИЭ в преклонном возрасте ассоциируется с плохим прогнозом и с высокой частотой осложнений.166,372,374,375 Это более тяжелое клиническое течение было связано со стертыми начальными симптомами и запоздавшим диагнозом у пожилых людей, и с более высокой частотой более агрессивных возбудителей в этой когорте.166,374,375
У пожилых пациентах желудочнокишечный источник инфекции был описан как ниболее частый. Группа D стрептококков (S. bovis) становится все более и более частая причиной ИЭ, особенно у пожилых,208,376 и ассоциируется с болезнью толстого кишечника, множественным клапанным вовлечением и высоким риком эмболии.208 ….Энтерококковый ИЭ, как показали, также был более частым у старших пациентов.377
Лихорадка - менее частая374 и анемия более частая у пожилых пациентов, вероятно связанная с высокой пропорцией S. bovis ИЭ, при котором повреждения толстого кишечника являются частыми и могут вызвать скрытое кровотечение.208 В некоторых исследованиях вегетации у пожилых, как сообщается, были меньше375 и несли более низкий риск эмболии.372 Не так давно отрицательные культуры крови наблюдались у 16.7% пожилых пациентов с ИЭ.69
Наконец, старший возраст был связан с плохим прогнозом в большинстве недавних исследований.166,372,374,375 Пожилые пациенты меньше лечатся хирургически, вероятно в связи с более высоким операционным риском, связанным с преклонным возрастом и частыми сопутствующими болезнями.378 Однако, хирургическое лечение представляется как разумный выбор у пожилых, с теми же самыми показаниями, что и у молодых пациентов.379
Часть 6. Инфекционный эндокардит во время беременности
Сложность беременной кардиолгической пациентки состоит в изменяющейся сердечно-сосудистой физиологии, которая может симулировать сердечные болезни и спутывать клиническую картину.380,381
Частота ИЭ во время беременности, как сообщали, была 0.006%.382 Поэтому, ИЭ при беременности чрезвычайно редок, и является или осложнением существующего ранее сердечного повреждения или
|
|
результатом внутривенного злоупотребления лекарствами. Материнская смертность приближается к 33%, большинство смертельных случаев связаны с СН или эмболией, в то время как эмбриональная смертность составляет 29%.382 Тщательное внимание должно быть обращено на любую беременную женщину с необъясненной лихорадкой и сердечным шумом. Быстрое обнаружение ИЭ и соответствующее лечение важно в сокращении риска и материнской и эмбриональной смертности.382
M. Ссылки
1. Moreillon P, Que YA. Infective endocarditis. Lancet 2004;363:139–149.
2. Habib G. Management of infective endocarditis. Heart 2006;92:124–130.
3. Horstkotte D, Follath F, Gutschik E, Lengyel M, Oto A, Pavie A, Soler-Soler J,
Thiene G, von Graevenitz A, Priori SG, Garcia MA, Blanc JJ, Budaj A,
Cowie M, Dean V, Deckers J, Fernandez Burgos E, Lekakis J, Lindahl B,
Mazzotta G, Morais J, Oto A, Smiseth OA, Lekakis J, Vahanian A, Delahaye F,
Parkhomenko A, Filipatos G, Aldershvile J, Vardas P. Guidelines on prevention,
diagnosis and treatment of infective endocarditis executive summary; the task
force on infective endocarditis of the European society of cardiology.
Eur Heart J 2004;25:267–276.
4. Naber CK, Erbel R, Baddour LM, Horstkotte D. New guidelines for infective
endocarditis: a call for collaborative research. Int J Antimicrob Agents 2007;29:
615–616.
5. Moulds RF, Jeyasingham MS. Antibiotic prophylaxis against infective endocarditis:
time to rethink. Med J Aust 2008;189:301–302.
6. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M,
Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL,
Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH,
Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT. Prevention of infective
endocarditis: guidelines from the American Heart Association: a guideline
from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki
Disease Committee, Council on Cardiovascular Disease in the Young, and
the Council on Clinical Cardiology, Council on Cardiovascular Surgery and
Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary
Working Group. Circulation 2007;116:1736–1754.
7. Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME,
Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM,
Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ,
Takahashi M, Taubert KA. Infective endocarditis: diagnosis, antimicrobial
therapy, and management of complications: a statement for healthcare professionals
from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki
Disease, Council on Cardiovascular Disease in the Young, and the Councils on
Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American
Heart Association: endorsed by the Infectious Diseases Society of
America. Circulation 2005;111:e394–e434.
8. Nishimura RA, Carabello BA, Faxon DP, Freed MD, Lytle BW, O’Gara PT,
O’Rourke RA, Shah PM. ACC/AHA 2008 Guideline Update on Valvular Heart
Disease: Focused Update on Infective Endocarditis. A Report of the American
College of Cardiology/American Heart Association Task Force on Practice
Guidelines. Circulation 2008;118:887–896.
|
|
9. Danchin N, Duval X, Leport C. Prophylaxis of infective endocarditis: French recommendations
2002. Heart 2005;91:715–718.
10. Gould FK, Elliott TS, Foweraker J, Fulford M, Perry JD, Roberts GJ, Sandoe JA,
Watkin RW, Working Party of the British Society for Antimicrobial C. Guidelines
for the prevention of endocarditis: report of the Working Party of the
British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2006;
57:1035–1042.
11. Naber CK, Al-Nawas B, Baumgartner B, Becker HJ, Block M, Erbel R, Ertl G,
Flu¨ckiger U, Franzen D, Gohlke-Ba¨rwolf C, Gattringer R, Graninger R,
Handrick W, Herrmann M, Heying R, Horstkotte D, Jaussi A, Kern P,
Kramer HH, Ku¨hl S, Lepper PM, Leyh RG, Lode H, Mehlhorn U, Moreillon P,
Mu¨gge A, Mutters R, Niebel J, Peters G, Rosenhek R, Schmaltz AA, Seifert H,
Page 36 of 45 ESC Guidelines
Shah PM, Sitter H, Wagner W, Wahl G, Werdan K, Zuber M. Prophylaxe der
infektio¨sen Endokarditis. Kardiologe 2007;1:243–250.
12. Richey R, Wray D, Stokes T. Prophylaxis against infective endocarditis: summary
of NICE guidance. BMJ 2008;336:770–771.
13. Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD,
Gaasch WH, Lytle BW, Nishimura RA, O’Gara PT, O’Rourke RA, Otto CM,
Shah PM, Shanewise JS. 2008 focused update incorporated into the ACC/
AHA 2006 guidelines for the management of patients with valvular heart
disease: a report of the American College of Cardiology/American Heart
Association Task Force on Practice Guidelines (Writing Committee to revise
the 1998 guidelines for the management of patients with valvular heart
disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society
for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons.
J Am Coll Cardiol 2008;52:e1–e142.
14. Hoen B, Alla F, Selton-Suty C, Beguinot I, Bouvet A, Briancon S, Casalta JP,
Danchin N, Delahaye F, Etienne J, Le Moing V, Leport C, Mainardi JL,
Ruimy R, Vandenesch F. Changing profile of infective endocarditis: results of a
1-year survey in France. JAMA 2002;288:75–81.
15. Hill EE, Herijgers P, Claus P, Vanderschueren S, Herregods MC, Peetermans WE.
Infective endocarditis: changing epidemiology and predictors of 6-month mortality:
a prospective cohort study. Eur Heart J 2007;28:196–203.
16. Tleyjeh IM, Abdel-Latif A, Rahbi H, Scott CG, Bailey KR, Steckelberg JM,
Wilson WR, Baddour LM. A systematic review of population-based studies of
infective endocarditis. Chest 2007;132:1025–1035.
17. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W,
Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ. Health
care-associated bloodstream infections in adults: a reason to change the
accepted definition of community-acquired infections. Ann Intern Med 2002;
137:791–797.
18. Tleyjeh IM, Steckelberg JM, Murad HS, Anavekar NS, Ghomrawi HM,
Mirzoyev Z, Moustafa SE, Hoskin TL, Mandrekar JN, Wilson WR,
Baddour LM. Temporal trends in infective endocarditis: a population-based
study in Olmsted County, Minnesota. JAMA 2005;293:3022–3028.
19. Letaief A, Boughzala E, Kaabia N, Ernez S, Abid F, Chaabane TB, Jemaa MB,
Boujnah R, Chakroun M, Daoud M, Gaha R, Kafsi N, Khalfallah A, Slimane L,
Zaouali M. Epidemiology of infective endocarditis in Tunisia: a 10-year multicenter
retrospective study. Int J Infect Dis 2007;11:230–233.
20. Nkomo VT. Epidemiology and prevention of valvular heart diseases and infective
endocarditis in Africa. Heart 2007;93:1510–1519.
21. Cabell CH Jr., Jollis JG, Peterson GE, Corey GR, Anderson DJ, Sexton DJ,
Woods CW, Reller LB, Ryan T, Fowler VG Jr. Changing patient characteristics
and the effect on mortality in endocarditis. Arch Intern Med 2002;162:90–94.
22. Fowler VG Jr, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, Corey GR,
Spelman D, Bradley SF, Barsic B, Pappas PA, Anstrom KJ, Wray D, Fortes CQ,
Anguera I, Athan E, Jones P, van der Meer JT, Elliott TS, Levine DP, Bayer AS.
Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA
2005;293:3012–3021.
23. Ribera E, Miro JM, Cortes E, Cruceta A, Merce J, Marco F, Planes A, Pare JC,
Moreno A, Ocana I, Gatell JM, Pahissa A. Influence of human immunodeficiency
virus 1 infection and degree of immunosuppression in the clinical characteristics
and outcome of infective endocarditis in intravenous drug users. Arch Intern Med
1998;158:2043–2050.
24. Hogevik H, Olaison L, Andersson R, Lindberg J, Alestig K. Epidemiologic aspects
of infective endocarditis in an urban population. A 5-year prospective study.
Medicine (Baltimore) 1995;74:324–339.
25. Berlin JA, Abrutyn E, Strom BL, Kinman JL, Levison ME, Korzeniowski OM,
|
|
Feldman RS, Kaye D. Incidence of infective endocarditis in the Delaware
Valley, 1988–1990. Am J Cardiol 1995;76:933–936.
26. van der Meer JT, Thompson J, Valkenburg HA, Michel MF. Epidemiology of bacterial
endocarditis in The Netherlands. I. Patient characteristics. Arch Intern Med
1992;152:1863–1868.
27. Aksoy O, Meyer LT, Cabell CH, Kourany WM, Pappas PA, Sexton DJ. Gender
differences in infective endocarditis: pre- and co-morbid conditions lead to
different management and outcomes in female patients. Scand J Infect Dis
2007;39:101–107.
28. Murdoch DR, Corey GR, Hoen B, Miro JM, Fowler VG Jr, Bayer AS,
Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH,
Falco V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF,
Utili R, Wang A, Woods CW, Cabell CH. Clinical presentation, etiology, and
outcome of infective endocarditis in the 21st century: the International Collaboration
on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009;169:
463–473.
29. Chu VH Jr., Cabell CH, Abrutyn E, Corey GR, Hoen B, Miro JM, Olaison L,
Stryjewski ME, Pappas P, Anstrom KJ, Eykyn S, Habib G, Benito N, Fowler VG
Jr. Native valve endocarditis due to coagulase-negative staphylococci: report
of 99 episodes from the International Collaboration on Endocarditis Merged
Database. Clin Infect Dis 2004;39:1527–1530.
30. Chu VH Jr., Woods CW, Miro JM, Hoen B, Cabell CH, Pappas PA, Federspiel J,
Athan E, Stryjewski ME, Nacinovich F, Marco F, Levine DP, Elliott TS, Fortes CQ,
Tornos P, Gordon DL, Utili R, Delahaye F, Corey GR, Fowler VG Jr. Emergence
of coagulase-negative staphylococci as a cause of native valve endocarditis. Clin
Infect Dis 2008;46:232–242.
31. Revilla A, San Roman JA, Lopez J, Vilacosta I, Luaces M, Fernandez-Aviles F.
Current profile of left-sided native valve endocarditis caused by coagulasenegative
Staphylococcus. Rev Esp Cardiol 2005;58:749–752.
32. Richardson DC, Burrows LL, Korithoski B, Salit IE, Butany J, David TE, Conly JM.
Tropheryma whippelii as a cause of afebrile culture-negative endocarditis: the
evolving spectrum of Whipple’s disease. J Infect 2003;47:170–173.
33. Croft LB, Donnino R, Shapiro R, Indes J, Fayngersh A, Squire A, Goldman ME.
Age-related prevalence of cardiac valvular abnormalities warranting infectious
endocarditis prophylaxis. Am J Cardiol 2004;94:386–389.
34. Que YA, Haefliger JA, Piroth L, Francois P, Widmer E, Entenza JM, Sinha B,
Herrmann M, Francioli P, Vaudaux P, Moreillon P. Fibrinogen and fibronectin
binding cooperate for valve infection and invasion in Staphylococcus aureus
experimental endocarditis. J Exp Med 2005;201:1627–1635.
35. Moreillon P, Overholser CD, Malinverni R, Bille J, Glauser MP. Predictors of
endocarditis in isolates from cultures of blood following dental extractions in
rats with periodontal disease. J Infect Dis 1988;157:990–995.
36. Strom BL, Abrutyn E, Berlin JA, Kinman JL, Feldman RS, Stolley PD, Levison ME,
Korzeniowski OM, Kaye D. Dental and cardiac risk factors for infective endocarditis.
A population-based, case–control study. Ann Intern Med 1998;129:
761–769.
37. Moreillon P, Que YA, Bayer AS. Pathogenesis of streptococcal and staphylococcal
endocarditis. Infect Dis Clin North Am 2002;16:297–318.
38. Fowler VG Jr, McIntyre LM, Yeaman MR, Peterson GE, Barth Reller L, Corey GR,
Wray D, Bayer AS. In vitro resistance to thrombin-induced platelet microbicidal
protein in isolates of Staphylococcus aureus from endocarditis patients correlates
with an intravascular device source. J Infect Dis 2000;182:1251–1254.
39. Okell CC, Elliott SD. Bacteraemia and oral sepsis: with special reference to the
aetiology of subacute endocarditis. Lancet 1935;226:869–872.
40. Glauser MP, Bernard JP, Moreillon P, Francioli P. Successful single-dose amoxicillin
prophylaxis against experimental streptococcal endocarditis: evidence for
two mechanisms of protection. J Infect Dis 1983;147:568–575.
41. Lockhart PB. The risk for endocarditis in dental practice. Periodontology 2000;23:
127–135.
42. Forner L, Larsen T, Kilian M, Holmstrup P. Incidence of bacteremia after
chewing, tooth brushing and scaling in individuals with periodontal inflammation.
J Clin Periodontol 2006;33:401–407.
43. Roberts GJ. Dentists are innocent! ‘Everyday’ bacteremia is the real culprit: a
review and assessment of the evidence that dental surgical procedures are a
principal cause of bacterial endocarditis in children. Pediatr Cardiol 1999;20:
317–325.
44. Duval X, Leport C. Prophylaxis of infective endocarditis: current tendencies,
continuing controversies. Lancet Infect Dis 2008;8:225–232.
45. Steckelberg JM, Wilson WR. Risk factors for infective endocarditis. Infect Dis Clin
North Am 1993;7:9–19.
46. Pallasch TJ. Antibiotic prophylaxis: problems in paradise. Dent Clin North Am
2003;47:665–679.
47. Duval X, Alla F, Hoen B, Danielou F, Larrieu S, Delahaye F, Leport C, Briancon S.
Estimated risk of endocarditis in adults with predisposing cardiac conditions
undergoing dental procedures with or without antibiotic prophylaxis. Clin
Infect Dis 2006;42:e102–e107.
48. Shanson D. New British and American guidelines for the antibiotic prophylaxis
of infective endocarditis: do the changes make sense? A critical review. Curr Opin
Infect Dis 2008;21:191–199.
49. Hall G, Hedstrom SA, Heimdahl A, Nord CE. Prophylactic administration of
penicillins for endocarditis does not reduce the incidence of postextraction bacteremia.
Clin Infect Dis 1993;17:188–194.
50. Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK.
Bacteremia associated with toothbrushing and dental extraction. Circulation
2008;117:3118–3125.
51. Lacassin F, Hoen B, Leport C, Selton-Suty C, Delahaye F, Goulet V, Etienne J,
Briancon S. Procedures associated with infective endocarditis in adults. A case
control study. Eur Heart J 1995;16:1968–1974.
52. Van der Meer JT, Van Wijk W, Thompson J, Vandenbroucke JP, Valkenburg HA,
Michel MF. Efficacy of antibiotic prophylaxis for prevention of native-valve endocarditis.
Lancet 1992;339:135–139.
53. Oliver R, Roberts GJ, Hooper L. Penicillins for the prophylaxis of bacterial endocarditis
in dentistry. Cochrane Database Syst Rev 2004:CD003813.
ESC Guidelines Page 37 of 45
54. Anderson DJ, Olaison L, McDonald JR, Miro JM, Hoen B, Selton-Suty C,
Doco-Lecompte T, Abrutyn E, Habib G, Eykyn S, Pappas PA, Fowler VG,
Sexton DJ, Almela M, Corey GR, Cabell CH. Enterococcal prosthetic valve infective
endocarditis: report of 45 episodes from the International Collaboration on
Endocarditis-merged database. Eur J Clin Microbiol Infect Dis 2005;24:665–670.
55. Lalani T Jr., Kanafani ZA, Chu VH, Moore L, Corey GR, Pappas P, Woods CW,
Cabell CH, Hoen B, Selton-Suty C, Doco-Lecompte T, Chirouze C, Raoult D,
Miro JM, Mestres CA, Olaison L, Eykyn S, Abrutyn E, Fowler VG Jr. Prosthetic
valve endocarditis due to coagulase-negative staphylococci: findings from the
International Collaboration on Endocarditis Merged Database. Eur J Clin Microbiol
Infect Dis 2006;25:365–368.
56. Chu VH, Sexton DJ, Cabell CH, Reller LB, Pappas PA, Singh RK, Fowler VG Jr,
Corey GR, Aksoy O, Woods CW. Repeat infective endocarditis: differentiating
relapse from reinfection. Clin Infect Dis 2005;41:406–409.
57. Renzulli A, Carozza A, Romano G, De Feo M, Della Corte A, Gregorio R,
Cotrufo M. Recurrent infective endocarditis: a multivariate analysis of 21 years
of experience. Ann Thorac Surg 2001;72:39–43.
58. Li W, Somerville J. Infective endocarditis in the grown-up congenital heart
(GUCH) population. Eur Heart J 1998;19:166–173.
59. Takeda S, Nakanishi T, Nakazawa M. A 28-year trend of infective endocarditis
associated with congenital heart diseases: a single institute experience. Pediatr
Int 2005;47:392–396.
60. Sherman-Weber S, Axelrod P, Suh B, Rubin S, Beltramo D, Manacchio J,
Furukawa S,Weber T, Eisen H, Samuel R. Infective endocarditis following orthotopic
heart transplantation: 10 cases and a review of the literature. Transpl Infect
Dis 2004;6:165–170.
61. Millar BC, Moore JE. Antibiotic prophylaxis, body piercing and infective endocarditis.
J Antimicrob Chemother 2004;53:123–126.
62. Yoshinaga M, Niwa K, Niwa A, Ishiwada N, Takahashi H, Echigo S, Nakazawa M.
Risk factors for in-hospital mortality during infective endocarditis in patients with
congenital heart disease. Am J Cardiol 2008;101:114–118.
63. Thilen U. Infective endocarditis in adults with congenital heart disease. Curr Infect
Dis Rep 2003;5:300–306.
64. Fernandez-Hidalgo N, Almirante B, Tornos P, Pigrau C, Sambola A, Igual A,
Pahissa A. Contemporary epidemiology and prognosis of health care-associated
infective endocarditis. Clin Infect Dis 2008;47:1287–1297.
65. Lockhart PB, Brennan MT, Fox PC, Norton HJ, Jernigan DB, Strausbaugh LJ.
Decision-making on the use of antimicrobial prophylaxis for dental procedures:
a survey of infectious disease consultants and review. Clin Infect Dis 2002;34:
1621–1626.
66. Martin MV, Longman LP, Forde MP, Butterworth ML. Infective endocarditis and
dentistry: the legal basis for an association. Br Dent J 2007;203:E1; discussion
38–39.
67. Prendergast BD. The changing face of infective endocarditis. Heart 2006;92:
879–885.
68. Thuny F, Di Salvo G, Belliard O, Avierinos JF, Pergola V, Rosenberg V, Casalta JP,
Gouvernet J, Derumeaux G, Iarussi D, Ambrosi P, Calabro R, Riberi A, Collart F,
Metras D, Lepidi H, Raoult D, Harle JR, Weiller PJ, Cohen A, Habib G. Risk of
embolism and death in infective endocarditis: prognostic value of echocardiography:
a prospective multicenter study. Circulation 2005;112:69–75.
69. Perez de Isla L, Zamorano J, Lennie V, Vazquez J, Ribera JM, Macaya C. Negative
blood culture infective endocarditis in the elderly: long-term follow-up. Gerontology
2007;53:245–249.
70. Sachdev M, Peterson GE, Jollis JG. Imaging techniques for diagnosis of infective
endocarditis. Infect Dis Clin North Am 2002;16:319–337, ix.
71. Greaves K, Mou D, Patel A, Celermajer DS. Clinical criteria and the appropriate
use of transthoracic echocardiography for the exclusion of infective endocarditis.
Heart 2003;89:273–275.
72. Petti CA Jr., Fowler VG Jr. Staphylococcus aureus bacteremia and endocarditis.
Cardiol Clin 2003;21:219–233, vii.
73. Evangelista A, Gonzalez-Alujas MT. Echocardiography in infective endocarditis.
Heart 2004;90:614–617.
74. Hill EE, Herijgers P, Claus P, Vanderschueren S, Peetermans WE, Herregods MC.
Abscess in infective endocarditis: the value of transesophageal echocardiography
and outcome: a 5-year study. Am Heart J 2007;154:923–928.
75. Vieira ML, Grinberg M, Pomerantzeff PM, Andrade JL, Mansur AJ. Repeated
echocardiographic examinations of patients with suspected infective endocarditis.
Heart 2004;90:1020–1024.
76. Chirillo F, Pedrocco A, De Leo A, Bruni A, Totis O, Meneghetti P, Stritoni P.
Impact of harmonic imaging on transthoracic echocardiographic identification
of infective endocarditis and its complications. Heart 2005;91:329–333.
77. Feuchtner GM, Stolzmann P, Dichtl W, Schertler T, Bonatti J, Scheffel H,
Mueller S, Plass A, Mueller L, Bartel T, Wolf F, Alkadhi H. Multislice computed
tomography in infective endocarditis: comparison with transesophageal echocardiography
and intraoperative findings. J Am Coll Cardiol 2009;53:436–444.
78. Raoult D, Casalta JP, Richet H, Khan M, Bernit E, Rovery C, Branger S, Gouriet F,
Imbert G, Bothello E, Collart F, Habib G. Contribution of systematic serological
testing in diagnosis of infective endocarditis. J Clin Microbiol 2005;43:5238–5242.
79. Tornos P, Iung B, Permanyer-Miralda G, Baron G, Delahaye F, Gohlke-Barwolf C,
Butchart EG, Ravaud P, Vahanian A. Infective endocarditis in Europe: lessons
from the Euro heart survey. Heart 2005;91:571–575.
80. Delahaye F, Rial MO, de Gevigney G, Ecochard R, Delaye J. A critical appraisal of
the quality of the management of infective endocarditis. J Am Coll Cardiol 1999;
33:788–793.
81. Baron EJ, Scott JD, Tompkins LS. Prolonged incubation and extensive subculturing
do not increase recovery of clinically significant microorganisms from standard
automated blood cultures. Clin Infect Dis 2005;41:1677–1680.
82. Lamas CC, Eykyn SJ. Blood culture negative endocarditis: analysis of 63 cases
presenting over 25 years. Heart 2003;89:258–262.
83. Brouqui P, Raoult D. New insight into the diagnosis of fastidious bacterial endocarditis.
FEMS Immunol Med Microbiol 2006;47:1–13.
84. Watkin RW, Lang S, Lambert PA, Littler WA, Elliott TS. The serological diagnosis
of staphylococcal infective endocarditis. J Infect 2006;53:301–307.
85. Millar BC, Moore JE. Current trends in the molecular diagnosis of infective endocarditis.
Eur J Clin Microbiol Infect Dis 2004;23:353–365.
86. Breitkopf C, Hammel D, Scheld HH, Peters G, Becker K. Impact of a molecular
approach to improve the microbiological diagnosis of infective heart valve endocarditis.
Circulation 2005;111:1415–1421.
87. Rovery C, Greub G, Lepidi H, Casalta JP, Habib G, Collart F, Raoult D. PCR
detection of bacteria on cardiac valves of patients with treated bacterial endocarditis.
J Clin Microbiol 2005;43:163–167.
88. Branger S, Casalta JP, Habib G, Collard F, Raoult D. Streptococcus pneumoniae
endocarditis: persistence of DNA on heart valve material 7 years after infectious
episode. J Clin Microbiol 2003;41:4435–4437.
89. Fenollar F, Raoult D. Molecular diagnosis of bloodstream infections caused by
non-cultivable bacteria. Int J Antimicrob Agents 2007;30 Suppl 1:S7–S15.
90. Fenollar F, Goncalves A, Esterni B, Azza S, Habib G, Borg JP, Raoult D. A serum
protein signature with high diagnostic value in bacterial endocarditis: results
from a study based on surface-enhanced laser desorption/ionization
time-of-flight mass spectrometry. J Infect Dis 2006;194:1356–1366.
91. Millar B, Moore J, Mallon P, Xu J, Crowe M, McClurg R, Raoult D, Earle J,
Hone R, Murphy P. Molecular diagnosis of infective endocarditis—a new
Duke’s criterion. Scand J Infect Dis 2001;33:673–680.
92. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis:
utilization of specific echocardiographic findings. Duke Endocarditis
Service. Am J Med 1994;96:200–209.
93. Fournier PE, Casalta JP, Habib G, Messana T, Raoult D. Modification of the diagnostic
criteria proposed by the Duke Endocarditis Service to permit improved
diagnosis of Q fever endocarditis. Am J Med 1996;100:629–633.
94. Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR.
Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis.
Clin Infect Dis 2000;30:633–638.
95. Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart
2004;90:611–613.
96. San Roman JA, Lopez J, Vilacosta I, Luaces M, Sarria C, Revilla A, Ronderos R,
Stoermann W, Gomez I, Fernandez-Aviles F. Prognostic stratification of patients
with left-sided endocarditis determined at admission. Am J Med 2007;120:369
e1–e7.
97. Chu VH, Cabell CH, Benjamin DK Jr, Kuniholm EF, Fowler VG Jr, Engemann J,
Sexton DJ, Corey GR, Wang A. Early predictors of in-hospital death in infective
endocarditis. Circulation 2004;109:1745–1749.
98. Hasbun R, Vikram HR, Barakat LA, Buenconsejo J, Quagliarello VJ. Complicated
left-sided native valve endocarditis in adults: risk classification for mortality. JAMA
2003;289:1933–1940.
99. Mansur AJ, Grinberg M, Cardoso RH, da Luz PL, Bellotti G, Pileggi F. Determinants
of prognosis in 300 episodes of infective endocarditis. Thorac Cardiovasc
Surg 1996;44:2–10.
100. Wallace SM, Walton BI, Kharbanda RK, Hardy R, Wilson AP, Swanton RH. Mortality
from infective endocarditis: clinical predictors of outcome. Heart 2002;88:
53–60.
101. Netzer RO, Altwegg SC, Zollinger E, Tauber M, Carrel T, Seiler C. Infective
endocarditis: determinants of long term outcome. Heart 2002;88:61–66.
102. Delahaye F, Alla F, Beguinot I, Bruneval P, Doco-Lecompte T, Lacassin F,
Selton-Suty C, Vandenesch F, Vernet V, Hoen B. In-hospital mortality of infective
endocarditis: prognostic factors and evolution over an 8-year period. Scand J
Infect Dis 2007;39:849–857.
103. Duval X, Alla F, Doco-Lecompte T, Le Moing V, Delahaye F, Mainardi JL,
Plesiat P, Celard M, Hoen B, Leport C. Diabetes mellitus and infective endocarditis:
the insulin factor in patient morbidity and mortality. Eur Heart J 2007;28:
59–64.
Page 38 of 45 ESC Guidelines
104. Jassal DS, Neilan TG, Pradhan AD, Lynch KE, Vlahakes G, Agnihotri AK,
Picard MH. Surgical management of infective endocarditis: early predictors of
short-term morbidity and mortality. Ann Thorac Surg 2006;82:524–529.
105. Castillo JC, Anguita MP, Ramirez A, Siles JR, Torres F, Mesa D, Franco M,
Munoz I, Concha M, Valles F. Long term outcome of infective endocarditis in
patients who were not drug addicts: a 10 year study. Heart 2000;83:525–530.
106. Wang A, Athan E, Pappas PA, Fowler VG Jr, Olaison L, Pare C, Almirante B,
Munoz P, Rizzi M, Naber C, Logar M, Tattevin P, Iarussi DL, Selton-Suty C,
Jones SB, Casabe J, Morris A, Corey GR, Cabell CH. Contemporary clinical
profile and outcome of prosthetic valve endocarditis. JAMA 2007;297:
1354–1361.
107. Revilla A, Lopez J, Vilacosta I, Villacorta E, Rollan MJ, Echevarria JR, Carrascal Y,
Di Stefano S, Fulquet E, Rodriguez E, Fiz L, San Roman JA. Clinical and prognostic
profile of patients with infective endocarditis who need urgent surgery. Eur
Heart J 2007;28:65–71.
108. Durack DT, Pelletier LL, Petersdorf RG. Chemotherapy of experimental streptococcal
endocarditis. II. Synergism between penicillin and streptomycin against
penicillin-sensitive streptococci. J Clin Invest 1974;53:829–833.
109. Wilson WR, Geraci JE, Wilkowske CJ,Washington JA 2nd. Short-term intramuscular
therapy with procaine penicillin plus streptomycin for infective endocarditis
due to viridans streptococci. Circulation 1978;57:1158–1161.
109a. Morris AJ, Drinkovic D, Pottumarthy S, MacCulloch D, Kerr AR, West T. Bacteriological
outcome after valve surgery for active infective endocarditis: Implications
for duration of treatment after surgery. Clin Infect Dis 2005;41:187–194.
110. Elliott TS, Foweraker J, Gould FK, Perry JD, Sandoe JA. Guidelines for the antibiotic
treatment of endocarditis in adults: report of the Working Party of the
British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2004;
54:971–981.
111. Westling K, Aufwerber E, Ekdahl C, Friman G, Gardlund B, Julander I, Olaison L,
Olesund C, Rundstrom H, Snygg-Martin U, Thalme A, Werner M, Hogevik H.
Swedish guidelines for diagnosis and treatment of infective endocarditis. Scand
J Infect Dis 2007;39:929–946.
112. Nicolau DP, Freeman CD, Belliveau PP, Nightingale CH, Ross JW, Quintiliani R.
Experience with a once-daily aminoglycoside program administered to 2,184
adult patients. Antimicrob Agents Chemother 1995;39:650–655.
113. Francioli P, Ruch W, Stamboulian D. Treatment of streptococcal endocarditis
with a single daily dose of ceftriaxone and netilmicin for 14 days: a prospective
multicenter study. Clin Infect Dis 1995;21:1406–1410.
114. Francioli P, Etienne J, Hoigne R, Thys JP, Gerber A. Treatment of streptococcal
endocarditis with a single daily dose of ceftriaxone sodium for 4 weeks. Efficacy
and outpatient treatment feasibility. JAMA 1992;267:264–267.
115. Sexton DJ, Tenenbaum MJ, Wilson WR, Steckelberg JM, Tice AD, Gilbert D,
Dismukes W, Drew RH, Durack DT. Ceftriaxone once daily for four weeks
compared with ceftriaxone plus gentamicin once daily for two weeks for treatment
of endocarditis due to penicillin-susceptible streptococci. Endocarditis
Treatment Consortium Group. Clin Infect Dis 1998;27:1470–1474.
116. Cremieux AC, Maziere B, Vallois JM, Ottaviani M, Azancot A, Raffoul H,
Bouvet A, Pocidalo JJ, Carbon C. Evaluation of antibiotic diffusion into cardiac
vegetations by quantitative autoradiography. J Infect Dis 1989;159:938–944.
117. Wilson AP, Gaya H. Treatment of endocarditis with teicoplanin: a retrospective
analysis of 104 cases. J Antimicrob Chemother 1996;38:507–521.
118. Venditti M, Tarasi A, Capone A, Galie M, Menichetti F, Martino P, Serra P. Teicoplanin
in the treatment of enterococcal endocarditis: clinical and microbiological
study. J Antimicrob Chemother 1997;40:449–452.
119. Moet GJ, Dowzicky MJ, Jones RN. Tigecycline (GAR-936) activity against Streptococcus
gallolyticus (bovis) and viridans group streptococci. Diagn Microbiol
Infect Dis 2007;57:333–336.
120. Levy CS, Kogulan P, Gill VJ, Croxton MB, Kane JG, Lucey DR. Endocarditis
caused by penicillin-resistant viridans streptococci: 2 cases and controversies
in therapy. Clin Infect Dis 2001;33:577–579.
121. Knoll B, Tleyjeh IM, Steckelberg JM, Wilson WR, Baddour LM. Infective endocarditis
due to penicillin-resistant viridans group streptococci. Clin Infect Dis 2007;
44:1585–1592.
122. Hsu RB, Lin FY. Effect of penicillin resistance on presentation and outcome of
nonenterococcal streptococcal infective endocarditis. Cardiology 2006;105:
234–239.
123. Shelburne SA 3rd, Greenberg SB, Aslam S, Tweardy DJ. Successful ceftriaxone
therapy of endocarditis due to penicillin non-susceptible viridans streptococci.
J Infect 2007;54:e99–101.
124. Martinez E, Miro JM, Almirante B, Aguado JM, Fernandez-Viladrich P,
Fernandez-Guerrero ML, Villanueva JL, Dronda F, Moreno-Torrico A,
Montejo M, Llinares P, Gatell JM. Effect of penicillin resistance of Streptococcus
pneumoniae on the presentation, prognosis, and treatment of pneumococcal
endocarditis in adults. Clin Infect Dis 2002;35:130–139.
125. Friedland IR Jr., McCracken GH Jr. Management of infections caused by
antibiotic-resistant Streptococcus pneumoniae. N Engl J Med 1994;331:
377–382.
126. Lefort A, Lortholary O, Casassus P, Selton-Suty C, Guillevin L, Mainardi JL. Comparison
between adult endocarditis due to beta-hemolytic streptococci (serogroups
A, B, C, and G) and Streptococcus milleri: a multicenter study in
France. Arch Intern Med 2002;162:2450–2456.
127. Sambola A, Miro JM, Tornos MP, Almirante B, Moreno-Torrico A, Gurgui M,
Martinez E, Del Rio A, Azqueta M, Marco F, Gatell JM. Streptococcus agalactiae
infective endocarditis: analysis of 30 cases and review of the literature,
1962–1998. Clin Infect Dis 2002;34:1576–1584.
128. Stein DS, Nelson KE. Endocarditis due to nutritionally deficient streptococci:
therapeutic dilemma. Rev Infect Dis 1987;9:908–916.
129. Lin CH, Hsu RB. Infective endocarditis caused by nutritionally variant streptococci.
Am J Med Sci 2007;334:235–239.
130. Cone LA, Sontz EM, Wilson JW, Mitruka SN. Staphylococcus capitis endocarditis
due to a transvenous endocardial pacemaker infection: case report and
review of Staphylococcus capitis endocarditis. Int J Infect Dis 2005;9:335–339.
131. Sandoe JA, Kerr KG, Reynolds GW, Jain S. Staphylococcus capitis endocarditis:
two cases and review of the literature. Heart 1999;82:e1.
132. Korzeniowski O, Sande MA. Combination antimicrobial therapy for Staphylococcus
aureus endocarditis in patients addicted to parenteral drugs and in nonaddicts:
a prospective study. Ann Intern Med 1982;97:496–503.
133. Cosgrove SE, Vigliani GA, Fowler VG Jr, Abrutyn E, Corey GR, Levine DP,
Rupp ME, Chambers HF, Karchmer AW, Boucher HW. Initial low-dose gentamicin
for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin
Infect Dis 2009;48:713–721.
134. Chirouze C, Cabell CH, Fowler VG Jr, Khayat N, Olaison L, Miro JM, Habib G,
Abrutyn E, Eykyn S, Corey GR, Selton-Suty C, Hoen B. Prognostic factors in 61
cases of Staphylococcus aureus prosthetic valve infective endocarditis from the
International Collaboration on Endocarditis merged database. Clin Infect Dis
2004;38:1323–1327.
135. Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE. Role of rifampin for
treatment of orthopedic implant-related staphylococcal infections: a randomized
controlled trial. Foreign-Body Infection (FBI) Study Group. JAMA 1998;279:
1537–1541.
136. O’Connor S, Andrew P, Batt M, Becquemin JP. A systematic review and
meta-analysis of treatments for aortic graft infection. J Vasc Surg 2006;44:38–45.
137. Riedel DJ, Weekes E, Forrest GN. Addition of rifampin to standard therapy for
treatment of native valve infective endocarditis caused by Staphylococcus
aureus. Antimicrob Agents Chemother 2008;52:2463–2467.
138. Howden BP, Johnson PD,Ward PB, Stinear TP, Davies JK. Isolates with low-level
vancomycin resistance associated with persistent methicillin-resistant Staphylococcus
aureus bacteremia. Antimicrob Agents Chemother 2006;50:3039–3047.
139. Fowler VG Jr, Boucher HW, Corey GR, Abrutyn E, Karchmer AW, Rupp ME,
Levine DP, Chambers HF, Tally FP, Vigliani GA, Cabell CH, Link AS,
DeMeyer I, Filler SG, Zervos M, Cook P, Parsonnet J, Bernstein JM, Price CS,
Forrest GN, Fatkenheuer G, Gareca M, Rehm SJ, Brodt HR, Tice A,
Cosgrove SE. Daptomycin versus standard therapy for bacteremia and endocarditis
caused by Staphylococcus aureus. N Engl J Med 2006;355:653–665.
140. Levine DP, Lamp KC. Daptomycin in the treatment of patients with infective
endocarditis: experience from a registry. Am J Med 2007;120:S28–S33.
141. Rose WE, Leonard SN, Sakoulas G, Kaatz GW, Zervos MJ, Sheth A,
Carpenter CF, Rybak MJ. Daptomycin activity against Staphylococcus aureus following
vancomycin exposure in an in vitro pharmacodynamic model with simulated
endocardial vegetations. Antimicrob Agents Chemother 2008;52:831–836.
142. Guignard B, Entenza JM, Moreillon P. Beta-lactams against methicillin-resistant
Staphylococcus aureus. Curr Opin Pharmacol 2005;5:479–489.
143. Vouillamoz J, Entenza JM, Feger C, Glauser MP, Moreillon P. Quinupristin–dalfopristin
combined with beta-lactams for treatment of experimental endocarditis
due to Staphylococcus aureus constitutively resistant to macrolide–
lincosamide–streptogramin B antibiotics. Antimicrob Agents Chemother 2000;44:
1789–1795.
144. Jacqueline C, Navas D, Batard E, Miegeville AF, Le Mabecque V, Kergueris MF,
Bugnon D, Potel G, Caillon J. In vitro and in vivo synergistic activities of linezolid
combined with subinhibitory concentrations of imipenem against methicillinresistant
Staphylococcus aureus. Antimicrob Agents Chemother 2005;49:45–51.
145. Perichon B, Courvalin P. Synergism between beta-lactams and glycopeptides
against VanA-type methicillin-resistant Staphylococcus aureus and heterologous
expression of the vanA operon. Antimicrob Agents Chemother 2006;50:
3622–3630.
146. Reynolds R, Potz N, Colman M, Williams A, Livermore D, MacGowan A. Antimicrobial
susceptibility of the pathogens of bacteraemia in the UK and Ireland
2001–2002: the BSAC Bacteraemia Resistance Surveillance Programme.
J Antimicrob Chemother 2004;53:1018–1032.
ESC Guidelines Page 39 of 45
147. Olaison L, Schadewitz K. Enterococcal endocarditis in Sweden, 1995–1999: can
shorter therapy with aminoglycosides be used? Clin Infect Dis 2002;34:159–166.
148. Gavalda J, Len O, Miro JM, Munoz P, Montejo M, Alarcon A, de la
Torre-Cisneros J, Pena C, Martinez-Lacasa X, Sarria C, Bou G, Aguado JM,
Navas E, Romeu J, Marco F, Torres C, Tornos P, Planes A, Falco V,
Almirante B, Pahissa A. Brief communication: treatment of Enterococcus faecalis
endocarditis with ampicillin plus ceftriaxone. Ann Intern Med 2007;146:574–579.
149. Das M, Badley AD, Cockerill FR, Steckelberg JM, Wilson WR. Infective endocarditis
caused by HACEK microorganisms. Annu Rev Med 1997;48:25–33.
150. Paturel L, Casalta JP, Habib G, Nezri M, Raoult D. Actinobacillus actinomycetemcomitans
endocarditis. Clin Microbiol Infect 2004;10:98–118.
151. Morpeth S Jr., Murdoch D, Cabell CH, Karchmer AW, Pappas P, Levine D,
Nacinovich F, Tattevin P, Fernandez-Hidalgo N, Dickerman S, Bouza E, Del
Rio A, Lejko-Zupanc T, de Oliveira Ramos A, Iarussi D, Klein J, Chirouze C,
Bedimo R, Corey GR, Fowler VG Jr. Non-HACEK gram-negative bacillus endocarditis.
Ann Intern Med 2007;147:829–835.
152. Houpikian P, Raoult D. Blood culture-negative endocarditis in a reference
center: etiologic diagnosis of 348 cases. Medicine (Baltimore) 2005;84:162–173.
153. Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol
Rev 2001;14:177–207.
154. Ellis ME, Al-Abdely H, Sandridge A, Greer W, Ventura W. Fungal endocarditis:
evidence in the world literature, 1965–1995. Clin Infect Dis 2001;32:50–62.
155. Garzoni C, Nobre VA, Garbino J. Candida parapsilosis endocarditis: a comparative
review of the literature. Eur J Clin Microbiol Infect Dis 2007;26:915–926.
156. Lye DC, Hughes A, O’Brien D, Athan E. Candida glabrata prosthetic valve endocarditis
treated successfully with fluconazole plus caspofungin without surgery: a
case report and literature review. Eur J Clin Microbiol Infect Dis 2005;24:753–755.
157. Lee A, Mirrett S, Reller LB, Weinstein MP. Detection of bloodstream infections
in adults: how many blood cultures are needed? J Clin Microbiol 2007;45:
3546–3548.
158. Tice AD, Rehm SJ, Dalovisio JR, Bradley JS, Martinelli LP, Graham DR, Gainer RB,
Kunkel MJ, Yancey RW, Williams DN. Practice guidelines for outpatient parenteral
antimicrobial therapy. IDSA guidelines. Clin Infect Dis 2004;38:1651–1672.
159. Andrews MM, von Reyn CF. Patient selection criteria and management guidelines
for outpatient parenteral antibiotic therapy for native valve infective endocarditis.
Clin Infect Dis 2001;33:203–209.
160. Monteiro CA, Cobbs CG. Outpatient management of infective endocarditis. Curr
Infect Dis Rep 2001;3:319–327.
161. Huminer D, Bishara J, Pitlik S. Home intravenous antibiotic therapy for patients
with infective endocarditis. Eur J Clin Microbiol Infect Dis 1999;18:330–334.
162. Aksoy O, Sexton DJ, Wang A, Pappas PA, Kourany W, Chu V, Fowler VG Jr,
Woods CW, Engemann JJ, Corey GR, Harding T, Cabell CH. Early surgery in
patients with infective endocarditis: a propensity score analysis. Clin Infect Dis
2007;44:364–372.
163. Vikram HR, Buenconsejo J, Hasbun R, Quagliarello VJ. Impact of valve surgery on
6-month mortality in adults with complicated, left-sided native valve endocarditis:
a propensity analysis. JAMA 2003;290:3207–3214.
164. Delahaye F, Celard M, Roth O, de Gevigney G. Indications and optimal timing for
surgery in infective endocarditis. Heart 2004;90:618–620.
165. Thuny F, Beurtheret S, Mancini J, Gariboldi V, Casalta JP, Riberi A, Giorgi R,
Gouriet F, Tafanelli L, Avierinos JF, Renard S, Collart F, Raoult D, Habib G.
The timing of surgery influences mortality and morbidity in adults with severe
complicated infective endocarditis: a propensity analysis. Eur Heart J 2009; in
press.
166. Di Salvo G, Thuny F, Rosenberg V, Pergola V, Belliard O, Derumeaux G,
Cohen A, Iarussi D, Giorgi R, Casalta JP, Caso P, Habib G. Endocarditis in the
elderly: clinical, echocardiographic, and prognostic features. Eur Heart J 2003;
24:1576–1583.
167. Habib G, Avierinos JF, Thuny F. Aortic valve endocarditis: is there an optimal
surgical timing? Curr Opin Cardiol 2007;22:77–83.
168. Piper C, Hetzer R, Korfer R, Bergemann R, Horstkotte D. The importance of
secondary mitral valve involvement in primary aortic valve endocarditis; the
mitral kissing vegetation. Eur Heart J 2002;23:79–86.
169. De Castro S, d’Amati G, Cartoni D, Venditti M, Magni G, Gallo P, Beni S,
Fiorelli M, Fedele F, Pandian NG. Valvular perforation in left-sided infective
endocarditis: a prospective echocardiographic evaluation and clinical outcome.
Am Heart J 1997;134:656–664.
170. Vilacosta I, San Roman JA, Sarria C, Iturralde E, Graupner C, Batlle E, Peral V,
Aragoncillo P, Stoermann W. Clinical, anatomic, and echocardiographic characteristics
of aneurysms of the mitral valve. Am J Cardiol 1999;84:110–113, A119.
171. Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA,
Rademakers FE, Marino P, Smiseth OA, De Keulenaer G, Leite-Moreira AF,
Borbely A, Edes I, Handoko ML, Heymans S, Pezzali N, Pieske B, Dickstein K,
Fraser AG, Brutsaert DL. How to diagnose diastolic heart failure: a consensus
statement on the diagnosis of heart failure with normal left ventricular ejection
fraction by the Heart Failure and Echocardiography Associations of the European
Society of Cardiology. Eur Heart J 2007;28:2539–2550.
172. Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL,
Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS,
Philbrick JT, Rakowski H, Thys DM. ACC/AHA/ASE 2003 guideline update for
the clinical application of echocardiography–summary article: a report of the
American College of Cardiology/American Heart Association Task Force on
Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines
for the Clinical Application of Echocardiography). J Am Coll Cardiol 2003;42:
954–970.
173. Kahveci G, Bayrak F, Mutlu B, Bitigen A, Karaahmet T, Sonmez K, Izgi A,
Degertekin M, Basaran Y. Prognostic value of N-terminal pro-B-type natriuretic
peptide in patients with active infective endocarditis. Am J Cardiol 2007;99:
1429–1433.
174. Miro JM Jr., Anguera I, Cabell CH, Chen AY, Stafford JA, Corey GR, Olaison L,
Eykyn S, Hoen B, Abrutyn E, Raoult D, Bayer A, Fowler VG Jr. Staphylococcus
aureus native valve infective endocarditis: report of 566 episodes from the International
Collaboration on Endocarditis Merged Database. Clin Infect Dis 2005;41:
507–514.
175. Bouza E, Menasalvas A, Munoz P, Vasallo FJ, del Mar Moreno M, Garcia
Fernandez MA. Infective endocarditis—a prospective study at the end of the
twentieth century: new predisposing conditions, new etiologic agents, and still
a high mortality. Medicine (Baltimore) 2001;80:298–307.
176. Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G,
Flachskampf F, Hall R, Iung B, Kasprzak J, Nataf P, Tornos P, Torracca L,
Wenink A. Guidelines on the management of valvular heart disease: the Task
Force on the Management of Valvular Heart Disease of the European Society
of Cardiology. Eur Heart J 2007;28:230–268.
177. Anguera I, Miro JM, Evangelista A, Cabell CH, San Roman JA, Vilacosta I,
Almirante B, Ripoll T, Farinas MC, Anguita M, Navas E, Gonzalez-Juanatey C,
Garcia-Bolao I, Munoz P, de Alarcon A, Sarria C, Rufi G, Miralles F, Pare C,
Fowler VG Jr, Mestres CA, de Lazzari E, Guma JR, Moreno A, Corey GR. Periannular
complications in infective endocarditis involving native aortic valves. Am J
Cardiol 2006;98:1254–1260.
178. Anguera I, Miro JM, San Roman JA, de Alarcon A, Anguita M, Almirante B,
Evangelista A, Cabell CH, Vilacosta I, Ripoll T, Munoz P, Navas E,
Gonzalez-Juanatey C, Sarria C, Garcia-Bolao I, Farinas MC, Rufi G, Miralles F,
Pare C, Fowler VG Jr, Mestres CA, de Lazzari E, Guma JR, Del Rio A,
Corey GR. Periannular complications in infective endocarditis involving prosthetic
aortic valves. Am J Cardiol 2006;98:1261–1268.
179. Daniel WG, Flachskampf FA. Infective endocarditis. In: Camm AJ, Lu¨scher TF,
Serruys PWeds. The ESC textbook of cardiovascular medicine. Oxford: Blackwell
Publishing; 2006. p671–684.
180. Leung DY, Cranney GB, Hopkins AP, Walsh WF. Role of transoesophageal
echocardiography in the diagnosis and management of aortic root abscess.
Br Heart J 1994;72:175–181.
181. Graupner C, Vilacosta I, SanRoman J, Ronderos R, Sarria C, Fernandez C,
Mujica R, Sanz O, Sanmartin JV, Pinto AG. Periannular extension of infective
endocarditis. J Am Coll Cardiol 2002;39:1204–1211.
182. Lengyel M. The impact of transesophageal echocardiography on the management
of prosthetic valve endocarditis: experience of 31 cases and review of
the literature. J Heart Valve Dis 1997;6:204–211.
183. Karalis DG, Bansal RC, Hauck AJ, Ross JJJ, Applegate PM, Jutzy KR, Mintz GS,
Chandrasekaran K. Transesophageal echocardiographic recognition of subaortic
complications in aortic valve endocarditis. Clinical and surgical implications. Circulation
1992;86:353–362.
184. Chan KL. Early clinical course and long-term outcome of patients with infective
endocarditis complicated by perivalvular abscess. CMAJ 2002;167:19–24.
185. Tingleff J, Egeblad H, Gotzsche CO, Baandrup U, Kristensen BO, Pilegaard H,
Pettersson G. Perivalvular cavities in endocarditis: abscesses versus pseudoaneurysms?
A transesophageal Doppler echocardiographic study in 118 patients
with endocarditis. Am Heart J 1995;130:93–100.
186. Anguera I, Miro JM, Vilacosta I, Almirante B, Anguita M, Munoz P, Roman JA, de
Alarcon A, Ripoll T, Navas E, Gonzalez-Juanatey C, Cabell CH, Sarria C,
Garcia-Bolao I, Farinas MC, Leta R, Rufi G, Miralles F, Pare C, Evangelista A,
Fowler VG Jr, Mestres CA, de Lazzari E, Guma JR. Aorto-cavitary fistulous
tract formation in infective endocarditis: clinical and echocardiographic features
of 76 cases and risk factors for mortality. Eur Heart J 2005;26:288–297.
187. Jenkins NP, Habib G, Prendergast BD. Aorto-cavitary fistulae in infective endocarditis:
understanding a rare complication through collaboration. Eur Heart J
2005;26:213–214.
188. Bashore TM Jr., Cabell C, Fowler V Jr. Update on infective endocarditis. Curr
Probl Cardiol 2006;31:274–352.
Page 40 of 45 ESC Guidelines
189. Manzano MC, Vilacosta I, San Roman JA, Aragoncillo P, Sarria C, Lopez D,
Lopez J, Revilla A, Manchado R, Hernandez R, Rodriguez E. [Acute coronary syndrome
in infective endocarditis]. Rev Esp Cardiol 2007;60:24–31.
190. Glazier JJ, Verwilghen J, Donaldson RM, Ross DN. Treatment of complicated
prosthetic aortic valve endocarditis with annular abscess formation by homograft
aortic root replacement. J Am Coll Cardiol 1991;17:1177–1182.
191. Knosalla C, Weng Y, Yankah AC, Siniawski H, Hofmeister J, Hammerschmidt R,
Loebe M, Hetzer R. Surgical treatment of active infective aortic valve endocarditis
with associated periannular abscess—11 year results. Eur Heart J 2000;21:
490–497.
192. Bishara J, Leibovici L, Gartman-Israel D, Sagie A, Kazakov A, Miroshnik E,
Ashkenazi S, Pitlik S. Long-term outcome of infective endocarditis: the impact
of early surgical intervention. Clin Infect Dis 2001;33:1636–1643.
193. Remadi JP, Habib G, Nadji G, Brahim A, Thuny F, Casalta JP, Peltier M,
Tribouilloy C. Predictors of death and impact of surgery in Staphylococcus
aureus infective endocarditis. Ann Thorac Surg 2007;83:1295–1302.
194. Thuny F, Avierinos JF, Tribouilloy C, Giorgi R, Casalta JP, Milandre L, Brahim A,
Nadji G, Riberi A, Collart F, Renard S, Raoult D, Habib G. Impact of cerebrovascular
complications on mortality and neurologic outcome during infective endocarditis:
a prospective multicentre study. Eur Heart J 2007;28:1155–1161.
195. Di Salvo G, Habib G, Pergola V, Avierinos JF, Philip E, Casalta JP, Vailloud JM,
Derumeaux G, Gouvernet J, Ambrosi P, Lambert M, Ferracci A, Raoult D,
Luccioni R. Echocardiography predicts embolic events in infective endocarditis.
J Am Coll Cardiol 2001;37:1069–1076
|
|
|
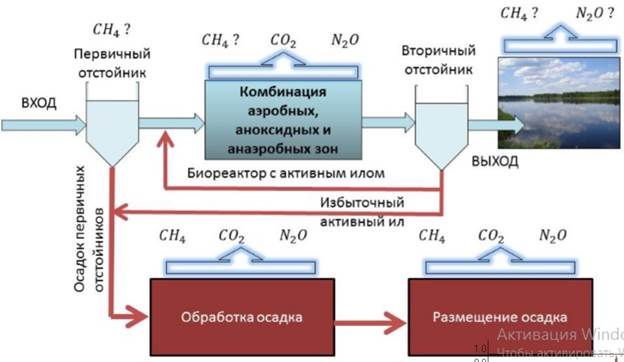
Эмиссия газов от очистных сооружений канализации: В последние годы внимание мирового сообщества сосредоточено на экологических проблемах...
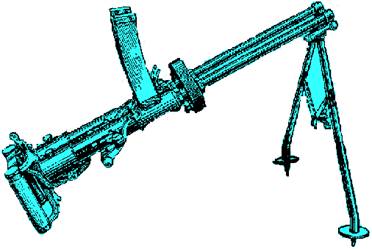
История развития пистолетов-пулеметов: Предпосылкой для возникновения пистолетов-пулеметов послужила давняя тенденция тяготения винтовок...
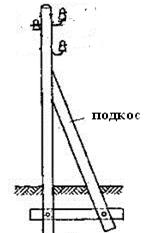
Опора деревянной одностоечной и способы укрепление угловых опор: Опоры ВЛ - конструкции, предназначенные для поддерживания проводов на необходимой высоте над землей, водой...
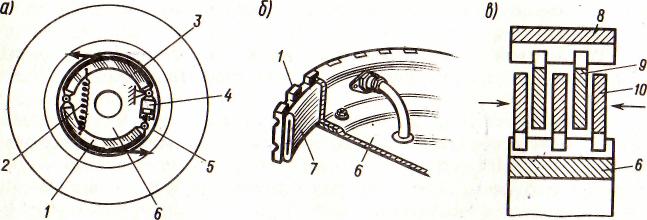
Автоматическое растормаживание колес: Тормозные устройства колес предназначены для уменьшения длины пробега и улучшения маневрирования ВС при...
© cyberpedia.su 2017-2024 - Не является автором материалов. Исключительное право сохранено за автором текста.
Если вы не хотите, чтобы данный материал был у нас на сайте, перейдите по ссылке: Нарушение авторских прав. Мы поможем в написании вашей работы!